Forum Replies Created
-
AuthorPosts
-
Don ColuzziSpectatorHi Ron: Both of my hygienists and I grew up on the pulsed Nd:YAG, and then we got our first diode, the ADT diolase when it first came out, I think about 4 or 5 years ago. That diode has only two buttons–one is CW and the other is a duty cycle of 50%, which is damn near like CW, especially when compared to pulsed Nd:YAG. So, to keep our heads on straight, we just learned to use the diode in CW, and the Nd:YAG as usual. You know that you have to work fast, but once you learn that, you can do quite well. So, pulsed diode works great for bacterial reduction, so if that’s what you learned, go for it, and you should be very successful! One thing to remember is that you’re not removing tissue when you’re preforming the procedure, rather you’re in a pool of blood and fluid. That liquid does act to disperse the heat, so CW isn’t really dangerous. The secret, of course is to get the photons to become absorbed. Hope this helps…….Keep Smilng………DON
SwpmnSpectator[img]https://www.laserdentistryforum.com/attachments/upload/williamsa073103-1.JPG[/img]
Hmmmmmm. Here’s what I found:
30Hz 255mJoules
25 355
20 375
10 355
3 200I’ll e-mail Tom this evening and ask for clarification. Is Glenn around this week?
Al
AlbodmdSpectatorLooks like you got more power than I Allen. I tried calibrating it and it was going up to 80, everything else seems to be ok. Wonder what’s different.
Al B
AnonymousSpectatorOk, who’s gonna do the glow in the dark golf after the luau, Friday?
2thlaserSpectatorme!
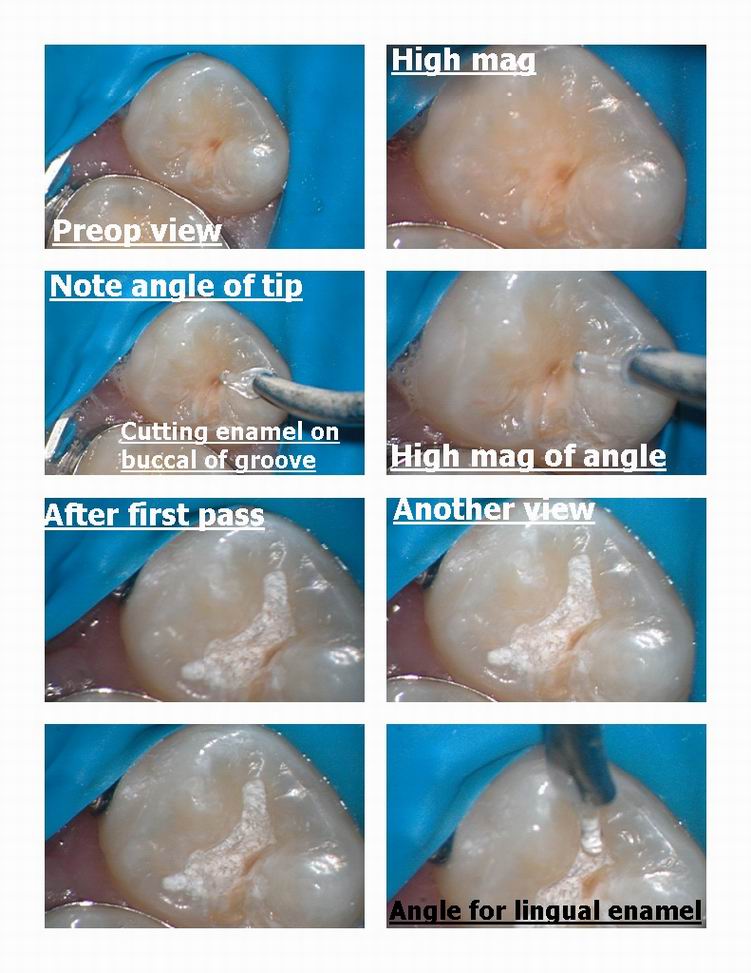
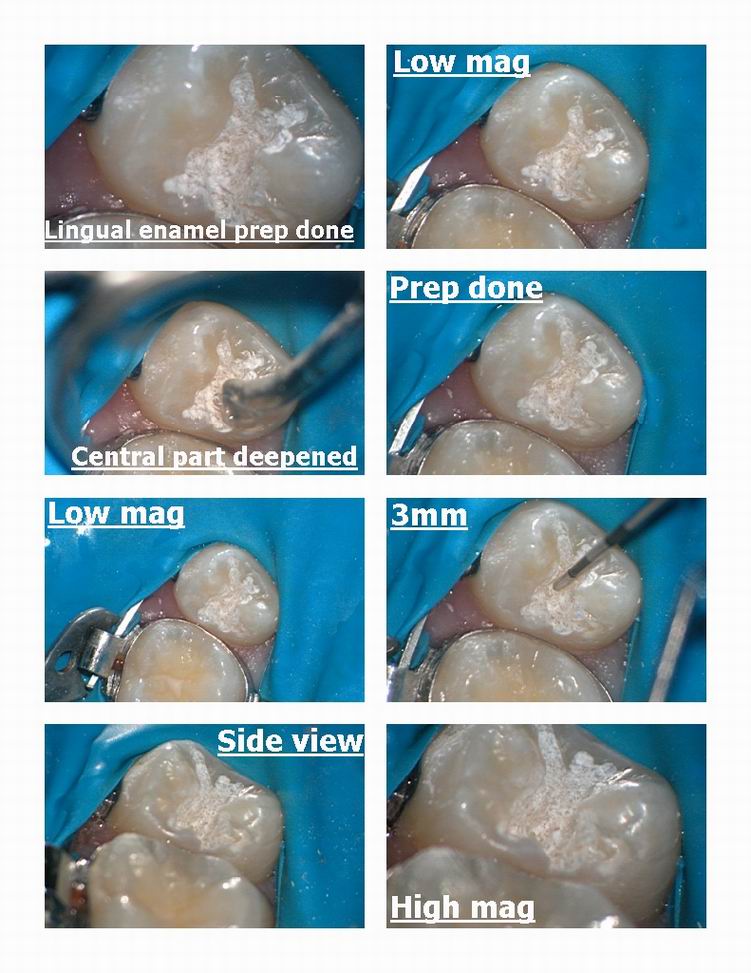
Glenn van AsSpectatorJust wanted to show a very easy case of how to do marks technique for occlusals on a patient.
Settings were 25 Hz and 240 mj , water on 600 micron tip ( could have used 400 but all mine were broken)
First pass buccal enamel rods on groove.
Second pass linqual enamel rods on groove,
Third pass central groove.
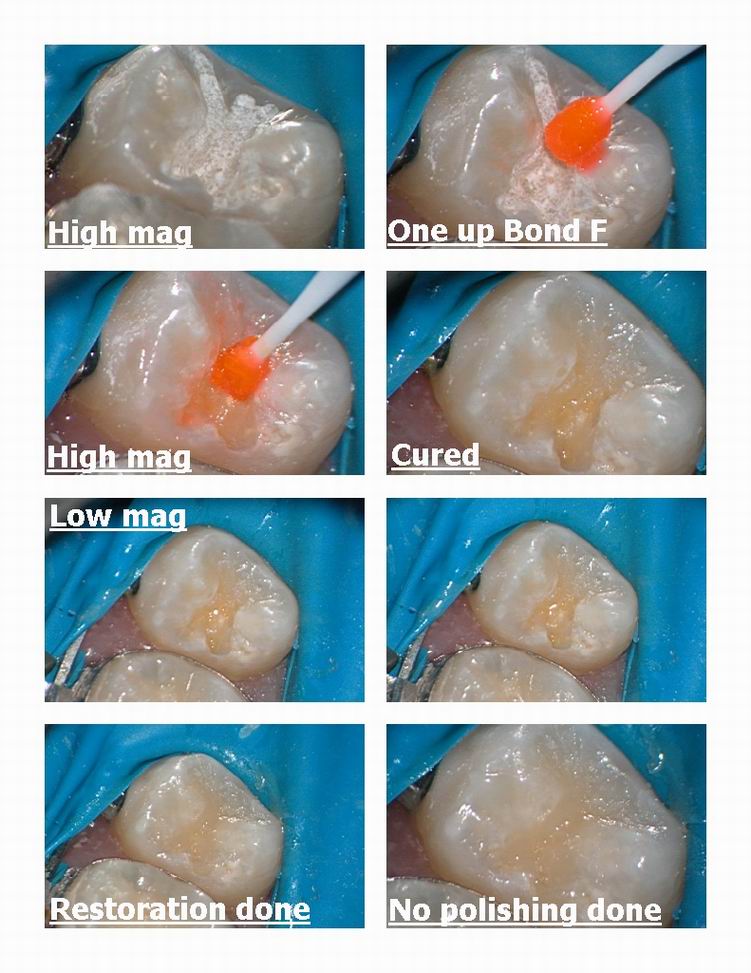
Used no etch bond ( J. Moritas one up bond F) to appease some here who hate to see phosphoric acid.
Used a new anterior spherical material Palfique A2 even though it was a premolar as it was in low function.
No polishing or adjustment done, all anatomy placed in with small felt instrument and optiquard placed. No polishing at all done.
Gotta go, simple case but still a case…..NO??
Glenn

Robert Gregg DDSSpectatorHi Guys,
Nice to see you posting Don. Great to see your expertise here!
Here’s an interesting poster presentation abstract from the American Association of Dental Research (AADR) meeting in San Antonio, March 12-15, 2003:
http://iadr.confex.com/iadr/2003SanAnton/techprogram/abstract_27983.htm
0855 Ablation of Porphyromonas gingivalis in vitro with Pulsed Dental Lasers
D.M. HARRIS, University of California, San Francisco, USA
Both pulsed Nd:YAG (1064nm)and continuous diode (810nm) dental lasers are in current use for treatment of periodontitis. It has been shown that laser treatment kills pathogenic bacteria (laser antisepsis), but a quantitative method for determining clinical dosimetry does not exist.
Objective: The purpose of this study was to develop a method to quantify the efficacy of ablation of Porphyromonas gingivalis (Pg) in vitro for two different lasers.
Methods: The ablation thresholds for the two lasers were compared in the following manner. The energy density was measured as a function of distance from the output of the fiber-optic delivery system. Pg cultures were grown on blood agar plates under standard anaerobic conditions. Blood agar provides an approximation of gingival tissue for the wavelengths tested in having hemoglobin as a primary absorber. Single pulses of laser energy were delivered to Pg colonies and the energy density was increased until the appearance of a small plume was observed coincident with a laser pulse. The energy density at this point defines the ablation threshhold.
Results: Ablation thresholds to a single pulse were determined for both Pg and for blood agar alone. The large difference in ablation thresholds between the pigmented pathogen and the host matrix for pulsed-Nd:YAG represented a significant therapeutic ratio and Pg was ablated without visible effect on the blood agar. At threshold the 810-nm diode laser destroyed both the pathogen and the gel.
Conclusion: Clinically, the pulsed Nd:YAG may selectively destroyed pigmented pathogens leaving the surrounding tissue intact. The 810-nm diode laser may not demonstrate this selectivity due to its greater absorption by hemoglobin.
My recollection from reading the poster is that pulsed Nd:YAG had a Therapeutic Ratio of Pg leathality of 24 to the 810 diode of 1.5. That’s a kill rate for pulsed Nd:YAG of Pg that is 16 times greater than CW/gated pulsed 810 diode–and at a depth of 2 mm into the tissues, whereas the CW/gated diode was a surface effect only.The reasons for this are simple:
1. True pulsed Nd:YAGs with pulse durations in the 100 millionth’s of a second, have peak powers of 1000-3000 watts per pulse. That’s also called intensity.
2. That sort of intensity with a near-infrared laser will penetrate the gingival tissues to at least a depth of 2 mm, and retain the light dose lethality sufficient to kill pathogens like Pg.
(Antibiotics penetrate only a few hundred microns)
3. Pg–one of the 3 main anaerobic pathogens associated with severe periodontitis and bone loss–is a black pigmented anaerobe that highly and selectively absorbs the 1064 nm Nd:YAG wavelength.
4. Pulse “off” times of 49,900 microseconds with pulsed Nd:YAGs allow for beam intensity “extinction” of the pulse intensity–and therefore thermal relaxation of the surrounding tissues, before the next bacteriacidal pulse of 100 microseconds is delivered.
CW/gated diodes neither have the selectivity, nor the forgiveness factor to the peripheral tissues, nor the intentisty for bacterial lethality to be the optimal device for the treatment of periodontal disease. But if it is all you’ve got, then it’s better than a hot papper clip for sulcular debridement and sulcular pathologic protein denaturization.
I prefer that the fiber be longer than the depth of the pocket–so we add a millimeter or 3. The rationale is that when a fiber breaks–as they do from time to time–the broken fiber will be sticking out of the sulcus.
The reason you want it shorter than the pocket depth measurement is when you are using the activated, “hot glass” effect using a diode in order to avoid charring the bone than is quick and certain when using the diode and contacting the bone.
Not so with a pulsed Nd:YAG. You can touch the bone (as long as you don’t hold it in place) and not have any adverse effects. In fact, one paper published (J Perio I think) stated that Nd:YAG in contact with bone stimulated bone regeneration where CO2 and erbium did not.
Just my 2 cents…..from an Old Fart!
Bob
2thlaserSpectatorVery very nice Glenn….simple, BUT that is what microdentistry is all about, and the laser is perfect for these applications. Again, the angulations of the tip to the enamel rods are so important to the speed of using the laser, you show that real well here. Thanks for showing what you do so often, we are so blessed to have you on this board Glenn.
Sincerely,
Mark
Glenn van AsSpectatorHad a new patient come in a 2 weeks or so ago after going to the oral surgeon and had a sharp point sticking out on the lingual of the #32 US (#48 international) and it cut the Heck out of his tongue.
WIthout local , using only topical (One touch and also Spray) I used the erbium without water at 30 Hz and 50 mj and then with water slightly to flush out the area and smooth it out.
He was so relieved and I was too to capture the offending piece.
The remaining solid bone was sharp on my finger so I smoothed it off a little with the laser.
He was ecstatic and really liked the fact that I could show him the case with the scope ( which helped me see it) and the laser which helped me remove it.
Neat case and easy without anesthetic needed.
Glenn
ASISpectatorHi Glenn,
Great documentation again.
But greater to see you back on the forum.
Andrew
ASISpectatorHi Glenn,
Was the bony spicule loose enough that you just flicked it out and smooth the edge off, or did you actually have to resect it with the laser and then smooth it?
Great documentation again. Thanks for sharing.
Andrew
whitertthSpectatorNice demo and nice restoration…. Do u routinely use that composite material…….Once again great stuff…I have been a little lazy posting lately but I will get back to it soon Regards to all..
whitertthSpectatorI’ll be glowing pretty good too…. Ron, my cell phone is 516 521 0394…call me on thursday ill be there around 6 ish…if anyone else wants to go to dinner speak now…we still have a few seats available at this AC hot spot….
AnonymousSpectatorRon,
Do you have the exact reservation time ( I don’t have any problem waiting for a late dinner if it means more can join the group)? Also, do you know how far the restaurant is from the hotel? I’ll also give you a call Thursday after 6, maybe we can share a cab to the restaurant.
Thanks for setting this up, I’m looking forward to putting some faces with the names of my friends here on the board!
Glenn van AsSpectatorHi guys: Here are the answers to your questions I hope
Mark , thanks , the scope is easy for documentation as I can just click away at will. Choose the best pics and save them in a patients folder. I now have a great remote on the camera and I am pretty happy with the results.
Andrew, thanks my friend for the comments. Its a simple case but all the same the pictures are able to add a level of understanding I think to any case that is shown. At times, there are things I wish I would do differently but there is always something positive to learn from any case.
Ron, thanks for the kind words. I am doing some work for Morita and chose to try that material out for this small posterior restoration. Palfique is intended for anterior situations but in this small occlusal and with her occlusion, there wasnt any contact.
I thought I would try it to see how it looked. It is spherical in particle shape and this supposedly allows it to be more translucent to the colors of the adjacent tooth structure. It is an ok material, I wonder how it compares to other nanocomposites and say Filtek supreme which are somewhat similar.
JUst posted the case to show you Marks technique. There was obviously no anesthetic used here as it was around 3 mm deep. Usually with phosphoric acid I can tell whether it was into the dentin or not (doesnt etch) but with the non etch bond, I cant tell.
In closing , I want to add that there is nothing wrong with constructive criticism on any case, its healthy to discuss alternative viewpoints. Its been the strength of the this forum, but it has always been my philosophy that if you want to throw rocks dont do so from glass houses.
Please feel free to post your cases here so we can learn from their strengths as well.
I think pictures are worth a thousand words, and I am fond of saying that magnified pictures are then worth 10,000 words……..
I do hope that many of you feel the same way.
Cheers
Glenn
-
AuthorPosts
