Forums › Laser Treatment Tips and Techniques › Hard Tissue Procedures › basic operative
- This topic is empty.
-
AuthorPosts
-
whitertthSpectatorJust some routine op. 5.5 watts no anaesthesia….filled with flowable…still used a 4 round buy for the leathery decay just to speed it up and finished with the laser. Patient didnt feel a thing



Glenn van AsSpectatorGood stuff Ron………..nice work.
How old was the patient ……around 11 or so?
I too use little round burs for caries removal, and then reuse the laser to remove the smear layer prior to etch and bond etc.
Good stuff.
Glenn
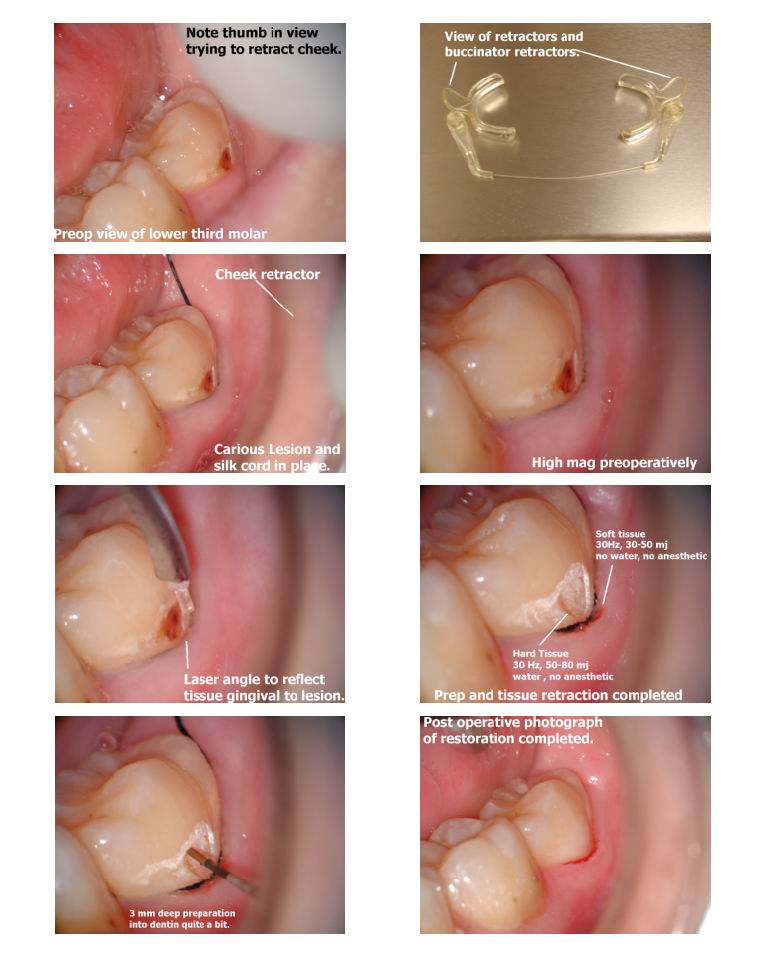
Glenn van AsSpectatorHere is a case I did simiilar in nature on a lower third molar . Man it is tough to see these but these retractors from J. Morita help. In addition I really like the pen grasp handpiece from Continuum as the access can be from the occlusal surface coming from the mesial.
With a handpiece or with the traditional handpiece laser the cheek really gets in the way ALOT.
I did this one as well without anesthetic and did the soft tissue as well.
HOpe you like it…………
Glenn
Glenn van AsSpectatorPS that photo collage was only 72 kb and done in Fotoslate with ACDSee. Saved it as a JPEG after it was complete.
Works great to give you one image only………..
Does it look ok to you guys and is this a good way to post a case…….I could actually get 24 pics into one case then if needed (3 photos with 8 photos per case)
Glenn
whitertthSpectatorgreat stuff…nice prep and nice restoration…… while i know some of the differences between the two lasers can u give me a quick rundown about the continuum…. thanks
whitertthSpectatorBTW, patient was 12 years old….
Glenn van AsSpectatorHi Ron: Here are some pics of the Continuum unit.
It is an Erbium Yag at 2940 nm and in addition has 5 pulse rates (Hz) of 3, 10,20, 25 and 30 Hz.
It is a fiber delivery system like Biolase and the fiber is very stable and very durable. It is 80 inches long.
There are two handpieces , a conventional handpiece like Biolase and a pen grasp handpiece which I use with the scope. They make a variety of shapes of tips, including standard 600 and 400 micron diameter quartz tips, endo tips, soft tissue tips, and as far as I am aware sapphire tips for the contra-angle handpiece.
It has a calibration port on the unit which allows for you to check weekly or so how the fiber is and it gives you a digital readout and when it gets to 65% you should replace it. Mine is still at 73% and it started at 80% 3 years ago.
THe water and air controls are just dials not % like the Biolase unit which I dont think is a strength on the continuum unit.
Its around 85 pds and has wheels. It can have either a direct air and water line or water bottle units with distilled water.
The maximum wattage is around 6 watts and the cost is around 39K.
I hope that helps you out somewhat.
Glenn[img]https://www.laserdentistryforum.com/attachments/upload/Resize of Rotation of DSCN2126.JPG[/img]
[img]https://www.laserdentistryforum.com/attachments/upload/Resize of DSCN2124.JPG[/img]
jetsfanSpectatorI have been using the waterlase for 2 years now and am amazed at some of the things that I can accomplish with it. That being said, I have some observations and a few questions for those able to do deep class 2’s w/o anesthesia on most patients in about the same time that it takes to do with anesthesia and a drill.
First, I am only successful approx 60% of time doing class 2 w/o anesth. , deep class 2’s much less successful than that. I often noticed patients really do feel it , too much for my comfort or theirs for that matter. I am able to do much of the prep but when it gets a little deep they start to complain. I have tried to reanesth. with the laser by several different methods, but once they feel it , they continue to feel it, even with Marks spoons or slow round bur. I have noticed that if I have 2 deep class 2’s back to back , I can do it more quickly, and with less pain by using anesth and a drill. ( I can use laser instead of drill and then the time improves).
Question, when you have the deep class 2, how gingerly do you progress axially? Are you aiming the tip from the interprox axially toward pulp or do you extend the occlusal portion and aim ginivally ?
Are your patients really feeling no pain or are tolerating it?
How much time do you schedule for those 2 class 2’s back to back?
I find that when they start to feel it , it becomes more stressful for me because I am trying to do it so they are comfortable. I then proceed more slowly and before I know it way too much time has elapsed and I am behind.
With anesth, I can be more aggressive removing caries. Am I the only one that notices these things?
Suggestions anyone. I was at Stu’s last year.
Thanks for your input.
Robert
kellyjblodgettdmdSpectatorRobert: I definitely hear what you are saying. I believe that I was doing class II’s without anes. roughly half of the attempts I made. Two things that have helped me achieve better success are: 1) I bought a microscope. I think the most significant effect this has had is that I can significantly reduce the power, but still see the laser working. I now rarely ever use Watt settings over 2.0W (this is with the Er,Cr:YSGG). 2) I do the most conservative prep possible, usually in the form of a tunnel prep or slot prep. I would say that since I started using the scope my class II percentage w/o anes. is maybe up to 85%. Some don’t feel it at all, whereas others say they do feel it, but is minor and they like not being numb. Of course, there are always those that are just jumpy and they don’t like to feel anything.
Also, I make a point of asking every patient I use the laser on which they like the least: the “shot” or feeling ANYTHING. I find that most patients would prefer to endure some mild to moderate stimulation of their nerve than to get the shot. However, those that simply don’t want to feel anything I have no problem getting them numb.
After using my Er laser for a year, I have decided that I just want patients to have a good experience. Generally, they will let me know what this looks like for them.
I don’t know if any of this helps. I’m sure you have tried everything I have to get better results. All I know is that every patient is different, and I think that has the most to do with the variability of results. Good luck!Kelly
dkimmelSpectatorRobert, What settings are you using as you get deep? By feel it on a scale of 1-10. what would you say they are feeling?
DAvid
jetsfanSpectatorI keep the power very low. They are feeling it at 1.75-2.25W 20%water 40-50% A.
This is with a g4, g6 or g9 tip, an of course I keep the tip moving. either from focus to defocus or side to side.
It seems all goes well, until they feel it. Then even if I attemp to reanesth, they will still feel it, with laser spoons or round bur. This problem seems to occur mostly ot the axial wall of moderately deep carious Cl 2 lesions. Cl 1,3,4 don’t seem to be as big a problem. Somehow I think it must be technique.
As an aside, David or anyone else; I am thinking of changing the name of my practice from Robert Tracey DDS to something like The Rockland Center for Laser and General Dentistry. What was reaction of your old time patients when they called.Were they asking if this was Dr Kimmel’s office? I assume you must have done some sort of mailing informing them of the name change.
Additonally, getting back to the class 2 ‘s. How much time would you schedule for a nervous adult with back to back class 2’s in the posterior, how about a fidgety 6 year old? I generally schedule an hour, but if they feel it I always run over.
Robert
ps. just got my lasersmile unit. I have used it for biostim and was pleasantly surprised.
drkddsSpectatorSo, Kelly, after you anesthetize the patient, do you use the handpiece or the laser?
In my experience, the majority of teeth needing anesthesia for laser tx are Cl. II lesions on premolars. It seems that any ablation directed pulpally is very sensitive, even at very low settings or using hand instruments or slow speed. Perhaps this is due to the relatively narrow M-D dimension at the cervical – proximity to the pulp.
I still use the laser after I anesthetize in most cases. Some patients just want to get out of the chair ASAP – so I use the handpiece on them.
kellyjblodgettdmdSpectatorHey, Doug. If a patient says that they’d rather be numb for the procedure, I still use the laser. I find that patients like not feeling all the vibration. Still, though, I almost always will finish w/ a new round bur with light pressure to finish the prep. And I restore any exposed dentin with auto-cure glass ionomer (Fuji IX). Since I started doing this over a year ago, I haven’t had a single case of post-op sensitivity. The enamel gets rebuilt w/ composite.
Kelly
jetsfanSpectator




Here is some basic laser dentistry. Nothing special. We all do this everyday. Just thought I’d share some nice pics.
Robert.p.s. How ’bout those Jets!
Glenn van AsSpectatorNice photos Robert and cool to see basic stuff.
I like the case and nice prep. On these I will do a couple of things…..
1. Isolate the adjacent tooth with a interquard.
2. Laser analgesia at 6 watts (30 Hz and 200 mj) for 2 mins on the distal marginal ridge but just defocussed at 4-10 mm
3. I will start the cavosurface outline in the enamel and prep that at high energy to try and build the outline before dropping into the decay.
4. drop the energy when I hit the denti and after a min or two use a round bur. I am careful with the laser to not go below the contact as this will always cause bleeding of the tissue. That is one reason I lower the energy to keep the laser from cutting too fast.
5. After the round bur slowspeed I take the laser back in at around 1.5 -2 watts to remove the smear layer and at the lower setting to put a cavosurface bevel on.That is how I would do these cases but everyone is different in their treatment. I am happy when others take the time to show their cases like you did Robert. It shows what the laser is capable of and that is fantastic.
Thanks for sharing.
Glenn
-
AuthorPosts
