Forums › Laser Resources › Laser Physics Related Literature › Dentistry Today Article
- This topic is empty.
-
AuthorPosts
-
AnonymousGuestIn case you hadn’t seen it. With permission (thanks Eric!)
Clinical protocols and quantum analysis for the use of Contact Sapphire Tips with the Er:YAG Dental Lasers on teeth and bone
Eric Bornstein, DMD
Introduction
From the first day of graduate dental education, prospective dentists are taught to think in terms of classical Newtonian mechanics. Dentists are taught about how mechanical work is produced from the force of a drill on a tooth, and about the heat that occurs (via friction), is a byproduct the drills motion on the tooth. (1,2) In short, dentists are generally taught about how things move , the forces that move them, and the thermodynamic consequences of these forces. These are accurate explanations for everyday experiences in dentistry, (3) however, these classical explanations are entirely superseded by systems reacting at minute atomic distances, and with system changes occurring at relativistic speeds (ie. the speed of light). In the science of laser-tissue interactions, the local environment follows an entirely different set of laws, called Quantum Mechanics. Also, with Er:YAG lasers, the thermodynamic equations that dentists are accustomed to (work producing heat) are reversed, and actually demonstrate heat (vaporized water) producing work. With quantum mechanics, we can make successful predictions for these new systems, at structures of atomic sizes and smaller, and for instantaneous velocities approaching the speed of light. (4) Laser dentists need to be aware of these different quantum rules, the reversed thermodynamic equations, and the logic behind them, so that they can make educated and proper judgments in treating patients with laser technology. Figure 1
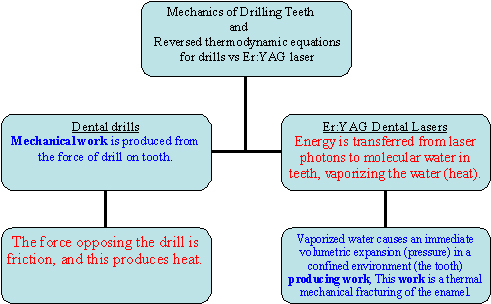
Figure 1: Difference between the Mechanics and Thermodynamics of Er:YAG
lasers and drillsWhen performing a procedure with Er:YAG lasers and contact sapphire tips, with the intention of cutting calcified biologic tissues (teeth and bone), a dentist will swiftly enter the extraordinary quantum world of very small distances between atoms and molecules. This is the case because Er:YAG laser photons (traveling at 300,000 kilometers/sec) uniquely target the chromophore of molecular water within the calcified biologic structure, and not the calcified structure itself. (5) Photon absorption by selected molecular chromophores in a biologic tissue (in this case water), with the concomitant quantum interactions, is the science of photobiology, and is a discipline that does not behave in a classical Newtonian manner. This scientific discipline of photobiology is largely unfamiliar to dentists, and attempts to explain the interactions of the nearly instantaneous transfer of quantized packets of energy (laser photons) to selected chromophores (absorptive molecules) in vital tissues. (5)
Photobiology and its quantum consequences, present many diverse and unusual issues to dental practitioners that need to be addressed with new explanations, and hence a laser dentist should have at least a perfunctory understanding of the quantum realm, if he/she is attempting to cut (ablate) calcified tissues (teeth and vital bone) with Er:YAG lasers. For example, the mechanics, interactions, and logic for cutting teeth and bone with lasers, is fundamentally different from that of using a conventional dental drill. With dental Er:YAG laser devices and contact tips, the prevailing logic is not simply,“ turn up the energy and push the tip harder against the tooth to cut faster”. The logic and mechanics of these devices do not follow the typical Newtonian thought progression that dentists generally use with drills (i.e “push the faster rotating bur with greater force against the tooth to obtain greater and faster cuts”). In actual fact, (as will be discussed presently) with Er:YAG lasers and contact tips, a dentist must learn to use an “up and down” motion, and to “back off” from a growing ablation crater (laser drilled hole), to accomplish safe and predictable cuts in calcified biologic tissues. This is the case, precisely because of certain quantum interactions at play. Only with an understanding of these quantum interactions can a laser dentist make quality intra-procedure decisions, based on the differences between the familiar Newtonian mechanics of drilling hard tissues with a handpiece, and the largely unfamiliar quantum mechanics of laser ablation of hard tissue with Er:YAG energy. (Figure 2 and 3)

Figure 2 Mechanical work produced from the drill

Figure 3
Thermal-Mechamical Ablation producing
work from vaporized waterthe Er:YAG
laser (Opus Duo, OpusDent USA)The purpose of this paper is to define and characterize clinical ablation (cutting) protocols with contact sapphire tips and Er:YAG lasers on calcified tissues, in an effort to maximize their safety, and ablation efficiency, with teeth and bone. This paper provides an explanation of many of the quantum realities at play at the laser-tooth crossing point, and provides a practical approach for avoiding what this author describes as the “quantum heat trap” effect, which is a thermodynamic event that produces a decrease in ablation efficiency. This can occur from excessive heat generation in a growing ablation crater of dental hard tissue, because of incorrect technique with Er:YAG irradiation, and contact sapphire tips.
Er:YAG lasers and water absorption
Atoms in a molecule are never at rest, and for each kind of a molecule (in this case water), there are what is known as normal vibration modes. For water molecules, there are three normal modes of vibration termed symmetric stretching, bending and assymmetric stretching. These vibration modes are entirely dependent upon the atomic geometry of the covalent bonds (–OH ) in the water molecules, and carry specific vibrational frequencies. (6) It is a known fact that the Er:YAG laser at a wavelength of 2.94µm has the highest specificity for water absorption of all the mid-infrared lasers, (7) and this is true, because one of the exact molecular vibration modes in the water molecule, generates a frequency that corresponds directly to the mid-infrared wavelength of of the Er:YAG laser at 2.94µm. (6) It is for this reason, that the absorption peak in water for Er:YAG energy is so high. (Figures 4 and 5)
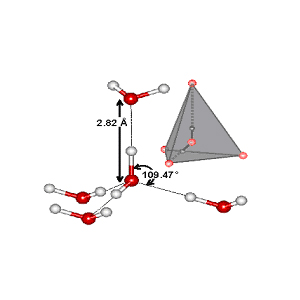
Figure 4 Tetrahedral Geometry of Water Molecule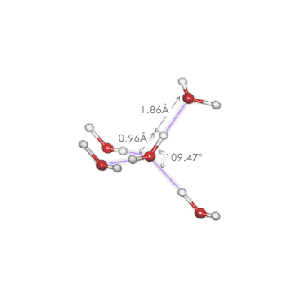
Figure 5 Hydrogen Bonds Between Water MoleculesImportance of Hydrogen bonds
The covalent (-OH) bonds in water molecules will bend and stretch, depending on the state of the hydrogen bonds between the water molecules. Hydrogen bonds are weak forces that attract water molecules to each other, and hence give water its property of cohesion. This facts are important because (as stated above) it is the vibrational modes in water molecules that are directly targeted by 2.94µm Er:YAG optical energy, and these vibrational modes are directly influenced by changes in the hydrogen bonds around the water molecules. For example, if the temperature of the water water is raised significantly, the hydrogen bonds attracting the water molecules to each other will weaken (and conversely the covalent –OH bonds will strengthen) changing the atomic geometry of the water molecules. Any geometric change in the molecule, will then alter the absorption peak for water (because the vibrational frequencies are also now altered), and this will make Er:YAG lasers less efficient tools. (6)
Hence, dental practitioners are dealing fully and entirely with the quantum interactions of 2.94µm optical energy, and the thermal and quantum changes that can occur to the target chromophore (molecular water), when using Er:YAG lasers. These quantum realities have enormous significance for the ablation (laser cutting) protocols practiced by dentists with these lasers, as an attempt must be made to keep the heat production to a minimum during ablation procedures, and hence prevent a negative shift in the absorption peak from occurring.Non-contact Hard Tissue Ablation with Er:YAG Lasers
Recently, a review of the literature presented that among the major clinical advantages of using an Er:YAG laser in dentistry, is it’s ability to ablate teeth and bone with minimal thermal damage. (8) The photobiology of the Er:YAG enamel interaction has been well defined in the past. (9,10,11) To review, water molecules within the prismatic enamel layer of a tooth make up only 4% of its chemical composition, however represent 11% of enamel’s total volume. As the laser Er:YAG energy interacts with the enamel matrix, water absorbs the laser energy and rapid vaporization of the water occurs. As this photothermal reaction takes place, the steam generated within the enamel is associated with a volumetric expansion and greatly increased pressure within the enamel matrix. This in turn produces microevaporative explosions that result in a thermally driven, mechanical ablation of the tooth structure. (11) A key finding in the past, has been the effect of water spray and thermal load on the ablation of calcified tissues. Specifically with teeth, Wigdor and Visuri (12,13) found that as long as enamel is continually hydrated with a water spray, during the laser exposure (serving as a heat sink), there will be only a minimal increase in temperature of the enamel layers and deeper tissues, as the ablation reaction continues. If we apply quantum mechanics to the above experimental findings, for the laser cutting of calcified tissue, what we are really observing is the mass action of a series of events, happening on an atomic scale, to large numbers of quantum objects. To further explain, it must be remembered that the Er:YAG laser photons are actually packets of optical energy striking a tooth. These quantized packets, in no way, shape, or form, behave in a classical Newtonian sense. Photons are not akin to colliding billiard balls, bullets, or rockets ballistically imparting a force on, and hence fracturing or abrading a tooth. (14) With all absorbed infrared light, after the energy of these (Er:YAG) photons is absorbed by the chrompohore (molecular water), it is converted to vibrational and rotational energy within the target molecules, which is the molecular basis for heat. It is this transfer of energy (into and vaporizing the water) that will cause, expansion and pressure in a confined environment (the tooth), leading to the explosive “thermal-mechanical ablation” of the tooth structure. (6)
With this quantum understanding, it has become the widely accepted view, that efficient ablation of biological tissues with pulsed Er:YAG lasers is always associated with a concomitant material ejection. This material ejection occurs via explosive phase transitions in the water that is embedded within the tissue matrix, and the speed of material ejection, and depth of the ablation crater production, appears to depend on the mechanical confinement strength of the extracellular tissue matrix (ie soft tissue or hard tissue, with hard tissue requiring more energy for adequate ablation and tissue ejection). (15, 16, 17, 18, 19)
Again, using the above reasoning to explain Wigdor and Visuri’s data, by continually hydrating the enamel of the irradiated teeth with water spray at the irradiation site, any significant temperature increase was kept to a minimum (ie the water spray acted as a heat sink), the negative shift in the absorption coefficient was prevented, and the water spray aided in washing away the boiling ejected material (products of ablation) enabling the reaction (thermal mechanical ablation) to continue smoothly.
Reviewing the medical literature, the same logic holds true for bone ablation with Er:YAG lasers. As many dental practitioners are currently using different commercially available erbium laser systems to cut bone during oral surgery, the results by Truong et al (20) investigating Er:YAG ablation of osseous nasal dorsum, should also be considered from a quantum perspective. Truong established that irradiating at 300 microsecond pulses and 10Hz, plus a continuous water spray on the area of irradiation during Er:YAG ablation of human nasal dorsum, resulted in the lowest level of thermal damage. Clinically, this study suggest that the same quantum heat considerations a dental clinician must be aware of when ablating teeth, is of equal or greater importance when cutting bone, because of its vital nature. To prevent a shift towards higher heat, and a negative absorption shift for water, the data suggest that a continuous water spray on the bony irradiation site acting as a heat sink, is the best way to avoid unwanted thermal sequelae.
Confirming the quantum reality that a cooling water spray directly on the ablation site prevent poor ablation and heat build up, are two experiments of note by Vodopyanov (21,22). They verified the effect of temperature on the absorption of Er:YAG laser radiation in water, and presented data that shows the peak 2.94µm absorption coefficient of water, will decrease as energy deposition (i.e. heat) from the laser increases, increasing the kinetic (vibrational) energy of the water, and hence weakening the hydrogen bonds. More recent data (Shori et al) (23) presents essentially the same picture for the Er:YAG/water interactions. Shori et al described the quantum mechanics of the water molecule under erbium laser irradiation and recently reported the following:
1) As water absorbs more of the incident energy of an Er:YAG laser, and the
temperature of the water increases, the length and strength of the OH bond
in the water molecule changes because of the large increase in kinetic energy.2) While this important phenomenon occurs the absorption peak for the water molecule shifts to wavelengths that are significantly shorter than 2.94µm.
3) The peak water absorption coefficient for Er:YAG photons at high laser
intensities (more energy and heat), drops to the equivalent of only 25% of the
water molecules’ original absorption ability at room temperature. This can
occur almost instantaneously as a lazed area heats up. This negative shift in
the absorption peak for water greatly diminishes ability of the beam to
perform thermal mechanical ablation of tissues. (23)All of these above data describing Er:YAG ablation dynamics, have profound clinical implications for the interaction of these lasers with mineralized dental tissues, and particularly with the use of contact energy delivery tips. For example, as the Shori conclusions are directly applicable to nonmineralized (soft) tissue, energy needed for hard tissue ablation will be greater, meaning the heat produced by the laser will be greater, and residual heat (from the ablation) will remain in the mineralized tooth or bone longer than what would occur for soft tissues. If a clinician is using a small diameter contact tip in an incorrect manner, and happens to imbed the tip within calcified tissue during material ablation (tooth or bone), a second negative quantum occurrence will transpire, that will fuel a marked heat increase to the system, and greatly inhibit further ablation. This second occurrence is based on the the Pauli exclusion principle of quantum mechanics, and is very important to avoid. (3,14)
Contact cutting of calcified tissues with Er:YAG lasers, and the
Pauli exclusion principle
It is now understood that an adequate supply of water directed to the target tissue, and the explosive ejection of boiling products of ablation, is of paramount importance for efficient Er:YAG ablation. This will avoid overheating, cracking, and melting of calcified biologic structures during the ablation, that can occur with either contact or non-contact energy delivery systems. However, as ablation (laser drilling) occurs in these tissues, and a crater forms, the quantum rules of the game that we have been following begin to change, and need to be addressed.
First, if an adequate water spray is not directed into the crater (the area of the laser-tooth interaction), a heat buildup at the tooth-beam interface will occur, and the products of ablation will start to accumulate. As the ablation crater becomes deeper, and less water is reaching the reaction, the deepest part of the crater will heat up considerably. This will occur almost immediately, if a contact tip is being used by a practitioner like a drill bit (i.e. the Newtonian thought of pushing it into a tooth like a rotating handpiece) and it becomes embedded in the ablation crater. To prevent this from occurring (embedding a contact tip in an ablation crater), a second quantum principle of contact laser ablation must be understood, so that the first principle of excess heat production weakening hydrogen bonds in the water, can be avoided. It is potentially at this point in a poorly performed contact tip ablation procedure, that the Pauli exclusion principle will present itself, and need to be dealt with. (3,14)
The Pauli exclusion principle is a fundamental rule of quantum mechanics that is just another way of stating the idea of impenetrability. This is to say that two things cannot occupy the same space at the same time. In other words, a piece of solid matter will keep out even the tiniest pieces of any other matter. If we apply this quantum principle to Er:YAG contact tip ablation of calcified solid tissues, the application of the law becomes clear. For example, if a small diameter (600 microns or less) contact sapphire tip (i.e. a solid piece of matter) becomes imbedded within the calcified structure being ablated (tooth or bone), an impermeable barrier will be formed around the tip. This occurs because the diameter of the tip increases in a cone-like pattern, from the apex of the tip (600 microns) to where it is held hooked into the laser handpiece (1000 microns). Once this happens, there is no longer any fresh water being allowed into the ablation crater because the tip is physically in the way, taking up the volume of the crater ( i.e the Pauli exclusion principle, that two things cannot occupy the same space at the same time). Also, the boiling material and ablation products, from the ablation reaction at the apex of the crater, cannot exit and be ejected from the crater for exactly the same reason; i.e the solid sapphire tip is now in the way. Figures 6 and 7
Figure 6 Water freely entering ablation area
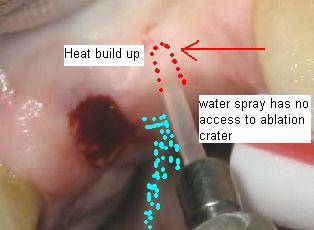
Figure 7 Tip embedded in ablation crater, with no room for removal of ablation products or water cooling sprayConcurrent with this problem, it is also important to remember that all lasers only deliver optical energy in one direction. In other words, they are end cutting devices, with ablation occurring in a straight directional vector from the end of the tip. When using a small diameter contact tip, the laser energy is more focused with a smaller spot size, and the laser beam will be intensified without ever increasing the power setting of the laser or the duration of application. This phenomenon can be explained with the following equation.
Power density (W/Cm² ) = Total power(W)/ Spot Size (Cm² )
This equation simply explains that the power density (brilliance) of the beam increases as the spot size of the beam becomes smaller. This makes available very precise and controlled ablation of teeth or bone in extremely small areas with the Er:YAG laser, but as a smaller ablation crater becomes deeper, it becomes increasingly difficult to inhibit the negative thermal sequale A dental laser practitioner must be aware of this, because if one of these solid sapphire tip becomes imbedded within a calcified tissue being cut and;
a) there is no water entering the crater,
b) there is no boiling ejected material leaving the creater (blowing off heat) .
c) the laser is still firing into the tissue, directly in a straight vector at the apex of
the crater;there will be a profound negative thermodynamic shift to the reaction, and ablation will stall. This author terms this phenomenon the “Quantum Heat Trap”.
The Quantum Heat trap
The quantum heat trap is by in large, an occurrence based on two different phenomena when using Er:YAG lasers with contact tips. The first is the clinical representation of the Pauli exclusion principle (discussed above), presenting as the completely blocked addition of exogenous water to the ablation site, and the “trapping” of the heat from the laser, as the boiling material ejection component of the ablation reaction, is prevented from exiting the ablation crater, by the physical volume of the solid sapphire contact tip. The second is the continuous deposition and “stacking” of the pulses from the laser into a concentrated area of the apex of the ablation crater, triggering a negative absorption shift for water to lower wavelengths. His is represented by the following animation. Figure # 8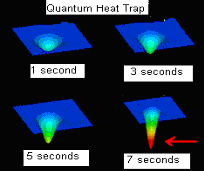
Figure 8
Thermal animation of continually firing
contact tip embedded in tissue resulting
in a quantum heat trapAnother way of describing the quantum heat trap can be found in research from Majaron et al in 1996 (24) , where they performed a threshold and efficiency analysis in Er:YAG laser ablation of hard dental tissue. Majaron et al described an interesting model of heat diffusion and ablation dynamics, and entered the term “ablation front” into the dental laser literature. The ablation front can be described as the physical distance, or depth into a solid structure, that the laser pulse will cause ablation. If the ablation front model is examined with quantum logic, it can now be understood that if the thermal front of the reaction (heat diffusion into the system from the laser) overtakes the ablation front of the reaction, (as could immediately happen with a continuously firing imbedded solid sapphire tip for the reasons previously discussed) a stall out effect in the ablation reaction will occur. So with any delivery system, contact or non- contact the operator is constantly attempting to keep the ablation front of the laser-tissue interaction ahead of the thermal front. However, with a contact tip delivery system, more careful technique and different thought processes are required.
Method to Avoid the Quantum Heat Trap
A practitioner using an erbium dental laser for hard tissue should never keep the contact energy delivery tip in one place on the tooth for more than 2-4 seconds at a time. Within the area to be cut by the laser, the practitioner should combine an up and down motion with a side to side motion at all times. Using these motions (instead of pushing the tip into the solid tissue like a bur) will prevent negative quantum interactions from taking place with these laser delivery systems. Theses recommendations, (fully against our typical Newtonian way of thinking with drills) will effectively allow;
1) the boiling products of ablation to explosively exit from a growing crater and
2) allow more water into the crater to act as a heat sink and flushing mechanism
Figure 9 and 10

Figure # 9 Up and down motion used for retrograde endodontic preparation
Figure # 10
Back off from ablation crater, allow the crater to cool, flush, and start again (OpusDuo, OpusDent USA)Without this approach, the thermal front of the Er:YAG-tooth ablation reaction will overtake the ablation front of the Er:YAG-tooth ablation reaction, and the result will be a negative heat buildup, a fall into the quantum heat trap with ablation “stall-out”, and negative sequalae will be experienced.
Morphological and Chemical Comparrison of contact Er:YAG laser cutting of bone to dental drills
Equivalence in morphological features and chemical composition of bone was documented experimentally by Sasaki (25) in his published study comparing contact bone cutting with an Er:YAG laser to a dental bur. In this study, Sasaki et al examined the bony surface after Er:YAG laser ablation at an output energy of 100mj/pulse in contact mode with an incident angle of approximately 30 degrees to the moistened surface of the bone under constant saline irrigation, at a pulse rate of 10Hz (1 W). Sites drilled using a conventional micromotor were used as controls at 10,000rpm, also with an angle of approximately 30 degrees, and constant saline irrigation. Analysis was completed using scanning electron microscopy (SEM) and Fourier transformed infrared (FTIR) spectroscopy . It was found that Er:YAG laser ablation (in the contact mode) produced a groove with similar dimensions to that produced by bur drilling. SEM observations revealed that the groove produced by the Er:YAG laser had well-defined edges and a smear layer-free surface with a characteristically rough appearance and with entrapped fibrin- like tissue. Additionally, the FTIR spectroscopy revealed that the chemical composition of the bone surface after contact Er:YAG laser ablation was much the same as that following bur drilling. The authors were able to show that Er:YAG contact laser irradiation with irrigation, at at 30 degree angle (presumably so as not to imbed the contact tip in the tooth) and bur drilling were essentially equivalent. Figures 11 and 12.

Figure 11 Alveoloplasty off angle 30 degrees with copious water spray on ablation site (OpusDuo, Opusdent USA)
Figure 12
Up and down handpiece motionThese results were essentially duplicated by Aoki et al in 2003 (26) . Both sets or researchers found substantial equivalence in bony cuts, morphological structure, and chemical composition of bone when cut with contact Er:YAG delivery systems, and continuous irrigation.
Conclusion
The following conclusions can be drawn from these discussions:
1)The conventional Newtonian mechanics associated with drilling hard dental tissues, including bone, must be superseded with non-traditional quantum mechanics, when drilling calcified structures with Er:YAG lasers in the contact mode.2)The target chromophore of water undergoes significant changes in its ability to further absorb Er:YAG laser radiation, if there is a large temperature change in the system being irradiated.
3)By changing the approach and protocol to “drilling” with Er:YAG lasers and contact tips, in clinical situations, the quantum heat trap leading to “stall out” can be avoided .
For the Er:YAG dental laser systems, a practitioner must make maximum use of a water spray focused on the ablation area. All available data and logic would preclude their use for so called “closed” or “flapless” surgical procedures for many of the quantum and thermodynamic reasons discussed above. If these systems are used with a side-to-side and up-and-down motions, always allowing copious irrigation on the site of ablation, it will promote the most efficient and least damaging ablation of tooth structure and bone when using contact energy delivery tips with these lasers..
Dr. Bornstein is a Biochemist that graduated from Tufts University School of Dental Medicine in 1992, and the Maimonides Medical Center General Practice Residency program in Brooklyn, NY in 1993. He has been using lasers in his dental practice since 1995, and practices general, implant, and laser dentistry in Natick, Massachusetts.
Disclosure: Dr. Bornstein is the Chief Science Officer for NOMIR Medical Technologies, a company focused on novel laser based solutions for biofilm eradication in dental and medical diseases. He is also consultant for OpusDent USA concerning matters of photobiology and laser tissue thermodynamics, and currently owns two combination Er:YAG/CO2 dual wavelength lasers and two 830nm diode lasers, all purchased from Opusdent USA. He also owns one 808nm Diode laser from ZAP Lasers USA.
Dr. Bornstein can be reached at drericdmd@mindspring.coReferences
1.Baum, L: Textbook of operative Dentistry, Second Edition, Philadelphia, W.B. Saunders Co., 1985.
2.Stannard, J: Materials in Dentistry, Second Edition, Hanover, Ma., Denali Publishing Co., 1988,
3. Serway, R.: Physics for Scientists and Engineers with Modern Physics, Second
Edition, Philadelphia, Saunders College Publishing, pp 93-95, and pp 991, 1986
4Hewitt, P: Conceptual Physics, Ninth Edition, San Francisco, Addison Wesley
Co., pp 496-635
5Niemz, M: Laser-Tissue Interactions. Fundamentals and Applications, Berlin,
Springer, 2002
6Ashley, J: Optical-Thermal Response Of Laser-Irradiated Tissue, New York, Plenum Press, pp 865-902, 1995.
7 Hale, G.M., Querry, M.R. (1973): Optical constants of water in the 200-nm to
200-um wavelength region. Appl. Opt. 12, 555-563
8Bornstein E. and Lomke M., Safety and Effectiveness of Dental Er:YAG Lasers:
A Literature Review with Specific Reference to Bone, Dentistry Today, Vol 22
No 10, pp129-133, October 2003
9. Walsh J, et al: Er:YAG Laser Ablation of Tissue: Effect of Pulse Duration
and Tissue Type on Thermal Damage, Lasers in Surgery and Medicine,
9:314-326,1989
10. Walsh J and Deutsch F, Er:YAG Ablation of Tissue: Measurement of
Ablation Rates, Lasers in Surgery and Medicine, 9:327-337,1989.
11 Moshonov J, Stabholz A, Leopold Y, et al: Lasers in dentistry. Part B—
Interaction with biological tissues and the effect on the soft tissues of the oral
cavity, the hard tissues of the tooth and the dental pulp. Refuat Hapeh
Vehashinayim 18(3-4):21-28, 107-8, 2001.
12. Wigdor, HA, Visuri, SR, Walsh, JT. Effect of water on dental material
ablation of the Er;YAG laser. SPIE Proc 1994
13.Visuri, SR, Walsh JT, Wigdor, HA. Erbium laser ablation of hard tissue:
Modeling and Control of the thermal load. SPIE Proc 1994;2128
14.Hey, T: The New Quantum Universe, Caimbridge, Caimbridge University Press,
pp1-15 and pp107-111, 2003.
15 Nahen K, Vogel A, Shielding by the ablation plume during Er:YAG laser
ablation,” in Laser-Tissue Interaction XII, vol. 4257, SPIE, 2001.
16 Hibst R, Keller U, Experimental studies of the application of the Er:YAG laser
on dental hard substances: I. Measurement of the ablation rate,” Lasers in
Surgery and Medicine, 9:338-344, 1989.
17Walsh JT, Deutsch TF, Measurement of Er:YAG laser ablation plume
dynamics,”Applied Physics B, 52:217{224, 1991.
18 Venugopalan V, Nishioka NS, Mikic BB, The thermodynamic response of soft
biological tissues to pulsed infrafred-laser irradiation,” Biophysical Journal,
70:2981-2993, 1996.
19 Marjaron B, Plestenjak P, Luka_c M, Thermo-mechanical laser ablation if soft
biological tissue: modeling the micro-explosions,” Applied Physics B, 69:71-80,
1999.
20 Truong, M. et al, Erbium:YAG Laser Contouring of the Nasal Dorsum: A
Preliminary Investigation. Lasers in Surgery: Advanced Characterization.
Therapeutics, and Systems XI, SPIE Vol. 4244, 2001
21Vodopyanov, KL., Bleaching water by intense light at the maximum of the lambda equqls 3 um Absorption band, Sov. Phys. JETP, 70: 114-121, 1990
22Vodopyanov, KL., Saturation studies of H2O and HDO near 3400 cm-1 using intense picosecond laser pulses, J. Chem Phys. 94: 5389-5393, 1991
23Shori et al, Quantification and Modeling of the Dynamic Changes in the Absorption Coefficient of Water at 2.94um. Journal on Selected Topics in Quantum Electronics, Vol 7, No 6, Nov/Dec 2001 pp959-970.
24Boris Majaron, B. et al, Threshold and efficiency analysis in Er:YAG laser
ablation of hard dental tissue, Laser Applications in Medicine and
Dentistry,SPIE Proceedings Vol. 2922, pp.233-242, 1996
25Sasaki KM, et al. Scanning Electron Microscopy and Fourier Transformed
Infrared Spectroscopy Analysis of Bone Removal using Er:YAG and CO2
Lasers. J Periontol 2002; 73:643-52
26Aoki A., Comparative study of Er:YAG laser and rotating bur for bone ablation,
International Congress Series 1248, pp389-391, 3003.Nice job on the article, Eric. (if you have better images as jpegs please email me).
dkimmelSpectatorNice to see Dentistry Today with some good Laser articles. Nice job Eric!
David
Glenn van AsSpectatorEric , it was a very interesting read, it jogged alot of thoughts on my part and I will have to read it agian
The literature that is mainstream needs articles like yours to make dentists aware of the necessity to get adequate training before or shortly after they purchase their product to use it to its maximum efficiency safely.
thanks for sharing it and wonderful stuff
Glenn
SwpmnSpectatorI’m not sure what the heck I just read, reminds me of the Spanish classses they forced me to take and barely passed to get in grad school.
From a clinical perspective:
1) Why would the operator want to contact hard, mineralized dental structures with an erbium laser tip? What are the advantages? The erbium lasers I use ablate hard tissues effectively out of contact at approximately 1mm. Is the proposal that the ablation is more efficient when used in contact? I did not find that at all in my extracted tooth experiences with the Opus Er:YAG system. Is the “Contact Concept” geared toward non-laser users which are accustomed to tactile feedback from a carbide/diamond bur in a high-speed handpiece?
2) Wouldn’t keeping an erbium laser tip out of contact with the substrate avoid all of the proposed negative sequelae? Heat buildup in the target site is avoided, the absorption spectrum shift of water molecules should be reduced and also the “ejecta” or products of ablation are efficiently washed away to facilitate the next ablation pulse of the erbium laser.
No disrespect is intended toward Dr. Bornstein but just seems to me that recommendations of “up and down” and “back off” indicate that ablation efficiency with an optical surgical instrument is best when used defocused or out of contact.
Al
michael simSpectatorThe shift of the absorption effectiveness shifting to a LOWER wavelength at HIGHER temperature may be the reason why the Biolase laser operates at a lower wavelength instead of the 2940nm we use. Does this also mean that the Er.YSGG laser MUST OPERATE AT A HIGHER TEMPERATURE? Will this therefore create potential thermal damage to the dental structures deeper beneath what we are cutting/ ablating ?
dkimmelSpectatorAllen, There is help! Lets get Al to present the paper this month at our meeting.
David
SwpmnSpectatorQUOTEThe shift of the absorption effectiveness shifting to a LOWER wavelength at HIGHER temperature may be the reason why the Biolase laser operates at a lower wavelength instead of the 2940nm we use. Does this also mean that the Er.YSGG laser MUST OPERATE AT A HIGHER TEMPERATURE? Will this therefore create potential thermal damage to the dental structures deeper beneath what we are cutting/ ablating ?I believe a study done by Daniel Fried indicated that a 2790nm erbium initiated enamel ablation at about 800 degrees Celsius while enamel ablation with a 2940nm erbium started at around 400 C.
Does this really translate into anything clinically as long as the treatment site is properly irrigated and cooled with water? In my opinion the answer is no. I use both wavelengths clinically and see no trend of the Er,Cr:YSGG erbium causing pulpitis/necrosis.
Al
Glenn van AsSpectatorBut it can cause the operators hair to fall out!!
Just kidding.
Glenn
SwpmnSpectatorQuote:But it can cause the operators hair to fall out!!/quote]Arf, arf, very funny.
At least my BMI(Body Mass Index) is below 27. It’s an obvious fact that use of the 2940nm erbium above the 49th parallel results in the operator developing a “spare tire”.
Al:wink:
SwpmnSpectatorFor some clinical feedback regarding the use of contact tips with erbium lasers:
This evening I had dinner with a local colleague who utilizes the Opus Duo(specific reference to the 2940nm Er:YAG). He relayed to me that he likes the contact tips because they give him the tactile sensation that we are so familiar with when using burs in a high speed handpiece. I’m still quite interested in any physical or tissue interaction advantages when erbium laser tips are used in contact. Can anyone help with their knowledge or perhaps propose a theory?
Al
SwpmnSpectatorFrom correspondence with the author of the paper, Eric Bornstein DMD:
1) Contact tips with erbium lasers afford the operator the advantage of the tactile sensation dentists are accustomed to while utilizing burs in dental handpieces. These contact tips have a narrower margin of error(heat buildup) when compared to erbium tips used in a defocused or out of contact mode. In order to avoid the negative sequelae of heat buildup at the ablation site, it is most important to only keep the tip in contact for one to two seconds and then back off from the treatment area. This was the purpose of the paper, to educate doctors using contact tips on proper technique and warn them not to keep pushing with an erbium tip like we do with a bur.
2) There are no physical or tissue interaction advantages with erbium laser contact tips. The purpose of the contact tip concept is simply to provide the clinician with tactile feedback. Dr. Bornstein added that he finds this particularly useful when performing apicoectomies and alveoplasty.
Al
AnonymousGuestHeads -up!
Coming in April (Dentistry Today)- CW near infrared Diode, and its use in Closed Periodontal Pocket procedures.This paper has more than 25 references from across the dental/medical spectrum, to help illustrate the points about “hot tips” in the closed environment of the periodontal pocket.
Soon as its in print it will be here also!
Thanks E.B.
Dentist2013SpectatorLasers are revolutionizing the dental and medical world as i think. Laser dentistry is fascinating, but for many of us it is confusing — access to information is limited because the cutting-edge technology is so new. Lasers may just revolutionize the way we practice dentistry and change the way we approach periodontal disease as a whole.
dentaltourismguideSpectatorThis is really great information article …
-
AuthorPosts
