- This topic is empty.
-
AuthorPosts
-
2thlaserSpectatorHey everyone,
Just wondering how everyone is using their laser for endo, Er, especially? Bob, Nd YAG? Can we share some thoughts? I have some ideas, and kind of want to begin a study on minimally invasive endo, which I think the laser needs to be a part of…From Mark on the Road back home!
Mark
AnonymousGuestMark, maybe by the overwhelming response, they’re not using the erbium much in endo
 ? 😉
? 😉What kind of study are you proposing?
dkimmelSpectatorMark, 100% of the time I will use the Waterlase as a last pass in the canal staying 3mm short of the apex .
Sometimes I will use the Waterlase to start my access just getting into the dentin or getting to the pulp chamber. I will then use burrs as I have a hard time getting a proper access without a tactile sense. ( Through the scope may change this)
Only once have I done endo without numbing the patient on a vital fractures tooth.Hope that helps
2thlaserSpectatorHi Ron, David,
I will post a couple of images here from Jim Jesse and his research from Loma Linda…..I am not sure I posted these before…here goes….
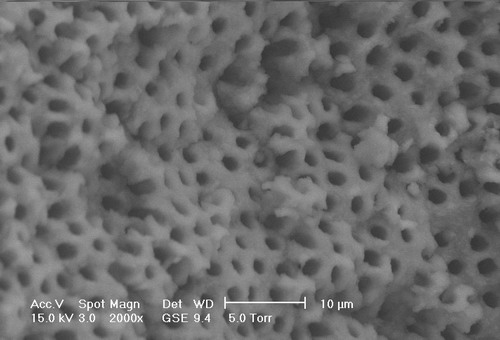
Here is SEM of Coronal, after tx with Er,Cr:YSGG 1W, 34/24 air/water:
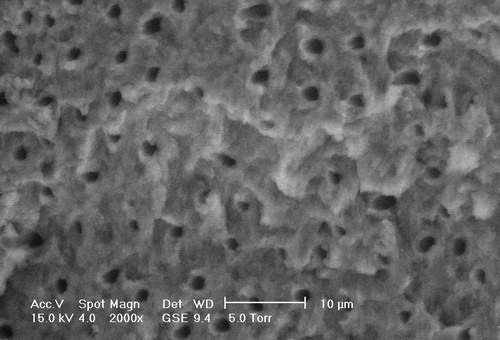
Here’s Middle 1/3: same settings
Here’s apex, same settings….note no smear layer, open tubules, no NaOCl, EDTA, just water/air/laser energy…
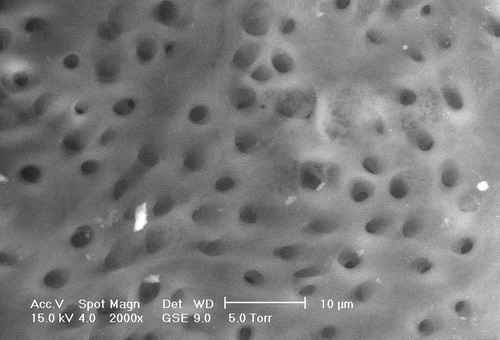
Thoughts on using laser instead of chemicals? Again, when time permits, I will show some cases, and explanations…..but I am collecting cases where minimally invasive techniques using the laser is key…
Mark
Vince C FavaSpectatorHi Mark,
I think lasers are a great adjunct to chemicals. In apices where there are accessory canals or arborization, I think that chemical soaks ideally in conjunction with ultrasonics are more predictable.
Regards
dkimmelSpectatorI still like chemicals. Primarly because of the last 3mm can be a crtical area. I do like finishing up with the laser just because of what those and other SEMs look like.
It can be tricky getting the waterflow and the laser to fire at the same time or at least delayed before the laser fires. I often find the laser fires and about the time I pull out the water starts to flow real well. Maybe I need to slow down but I fell uncomfortable firing an end cutting laser in a small closed space with no air/water.
kellyjblodgettdmdSpectatorMark – good thread. The challenge I find in consistently using the YSGG for endo is that the canals are often too small to allow their use. So then I’m stuck with a minimally invasive dilemma: Do I size up the canal so that I can get a Z2 tip down there, or do I just leave it where it is and rinse a little while longer? In my practice, it seems like the vast majority of RCTs I do are on 1st and 2nd molars, and frequently the buccal canals are just too small.
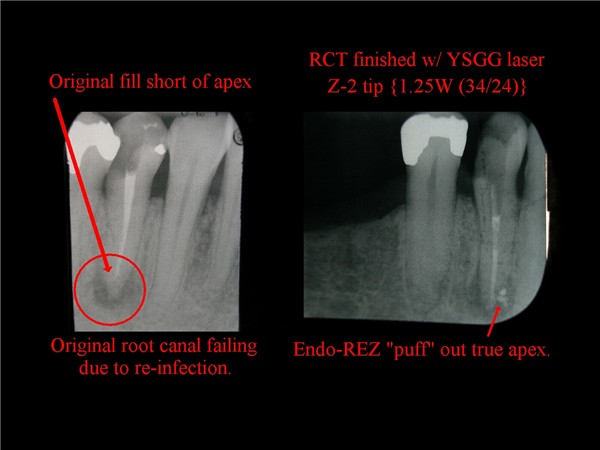
That being said, I sure do like using it when I can. As in this case of re-treating this root canal. It sure helped in opening up the five or so accessory canals.
Kelly
2thlaserSpectatorKelly,
Nice case. One very important thing to remember is that you get a “shotgun” effect of laser energy past the tip. We used to think 3mm short of the apex was sufficient to not have the energy blow out the end of the root, but I think we were wrong. I think it’s more like 4mm. That is another reason a Z-2 fiber doesn’t have to go all the way to the working length, and one can prepare a tooth with minimally invasive technique. So far, studies have shown (Jesse), that 1.5W, 20hz, 34/24air/water and at least SEVEN passes out the canal can give you a 98.6 kill rate of the bacterial contents….here is a graphic of how the energy dissiapates out of the tip of a Z-2 fiber….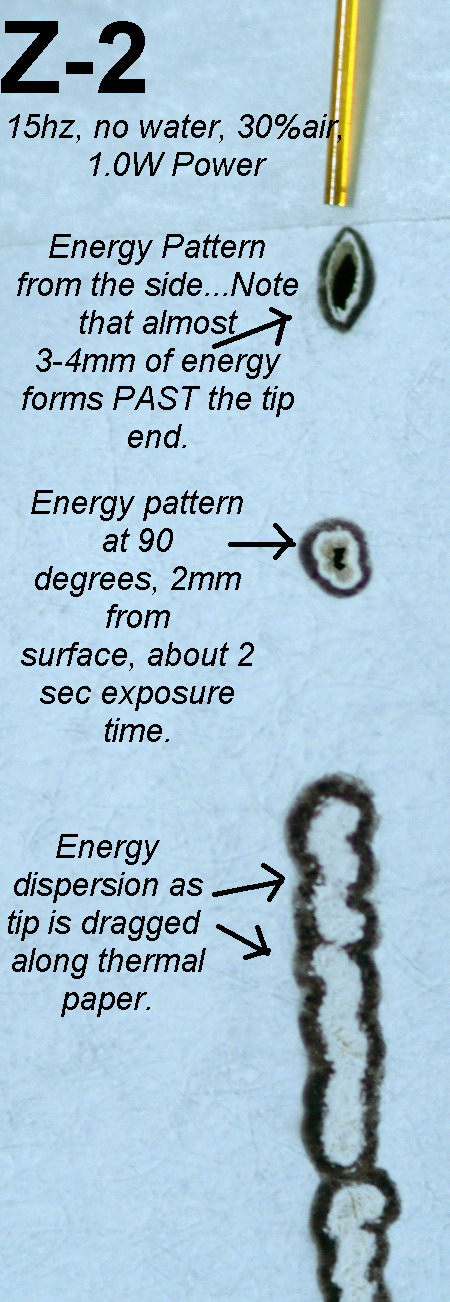
Note the energy we don’t “see” from doing this on thermal paper, is transmitted beyond the tip. Yes, there is some absorption of energy, but we see more “shotgun” like overfills for this very reason. Again, I think we need to be at least 4mm from the working length rather than 2 or 3 as previously thought, especially using 1.5W of energy in a 200micron tip…
Thoughts?

Mark
kellyjblodgettdmdSpectatorMark – I am glad to hear this from you. Since I started using the YSGG for RCTs 2 years ago, I found out very quickly that being 4-5mm from the apex often gave me much better comfort, and gave the patient greater comfort, too. Realistically, there’s no way that the air and water that are coming out of the handpiece are getting to the apex. Therefore, I am extremely cautious in the apical third when using the laser. I will often use 0.75W (34/24), but do 12 passes so that the total amount of joules is the same. Also, when using a little less energy per pulse, I feel more comfortable if I happen to encroach a little more closely than 4mm. Just my thoughts.
Kelly
Glenn van AsSpectatorHere is something to ponder as you get further and further away from the apex……….this is what worries me.
I am concerned that the laser without a non cutting tip (ie blocked like the OPUS tip) may never be as good as some of the irrigating canulas that are being introduced in endo that allow side irrigation. We need this for endo.
Here is the article……read the conclusions……and ponder.
Glenn
Aust Endod J. 2004 Apr;30(1):20-2.
Evaluation of the antimicrobial effect of Er:YAG laser irradiation versus 1% sodium hypochlorite irrigation for root canal disinfection.
Perin FM, Franca SC, Silva-Sousa YT, Alfredo E, Saquy PC, Estrela C, Sousa-Neto MD.
Faculty of Dentistry, Universidade de Ribeirao Preto, Ribeirao Preto, Sao Paulo, Brazil.
This laboratory study evaluated Er:YAG laser antibacterial action in infected root canals. Forty-eight maxillary central incisors were used. After canal preparation, the teeth were autoclaved and divided into four groups: (1) non-treated teeth (control group); (2) teeth treated with NaOCl; (3) teeth irradiated with Er:YAG laser (7 Hz, 100 mJ, 80 pulses/canal, 11 sec) to the working length; (4) teeth irradiated similarly to, but 3 mm short, of the apex. The root canals from Groups 2, 3 and 4 were inoculated with 4 bacteria: Bacillus subtillus, Enterococcus faecalis, Pseudomonas aeruginosa, and Staphylococcus aureus, together with Candida albicans, and maintained for 24 h at 37 degrees C. All suspensions were adjusted to tube 2 of the MacFarland scale. The intracanal material was then collected with sterile paper points, which were placed in the canals for 5 min and then immersed in 5 ml of BHI medium. This was then seeded onto agar and stained by Gram’s method. The NaOCl solutions and the Er:YAG laser irradiation to working length were effective against all five micro-organisms; however, 70% of the specimens irradiated 3 mm short of the apex remained infected.
PMID: 15116905 [PubMed – indexed for MEDLINE]
whitertthSpectatorInteresting article…,maybe the answer is going to the apex with the nergy at all times with all lasers……..and if we have energy going past the apex..it may not be bad in killing bacteria in the periapical area….I’m not so sure that we are not too far away from”Intracanal access to apicoectomies”….
Lee AllenSpectatorIn trying to place the clinical results with the lab study, I wonder if we are mixing apples and oranges.
In the Brazilian study, the energy used is less than the YSGG protocol and these results are on a different machine.
Glenn, is there a difference in the OPUS tips and energy delivery than the clad Z tips for the Waterlase? Aren’t they both end delivery systems?
Jesse’s ESM suggests there is no need to travel the last 3 mm to get bacterial elimination at a higher energy level.
I would suggest, as a conclusion, that if one approaches the apical end and does not want to affect the hard tissue profile, the necessary ingredients are water in the canal end and low energy that will allow decontamination.
What settings would be appropriate for the Waterlase at 20 not 7 Hz. 80 pulses is a short time (11 seconds) for the YAG overall if multiple passes are the technique du jour. Or in the study is this stationary? Watts being Hz times joules would mean the lowest Waterlase Classic setting possible is .25 watts at 20 Hz which equals 125 mj each second. Very low compared to conventional Waterlase recommended and studied settings.
I do not have an answer, just looking for some reasonable explainations.
Glenn van AsSpectatorHi Lee: great comments, very well thought out and I only have some answers for you with respect to the energy.
If in fact the old Waterlase has only a 20 Hz reading that would mean to get .25 watts the mj would be 12.5 mj (not 125 which would be 2.5 watts).
(20 and 12.5 divided by 1000 is .25 watts)
Now as for the rest of your questions. I think it is very astute that if you are going to the apex that you try to use as little energy as possible at the apex to avoid opening up the foramen. Question is what is the lethal kill rate for bacteria from an energy standpoint.
The tips for the DeLight are either 200 or 300 microns wide and the maximum energy for them is only 2 watts.
I myself can only use a minimum of .3 hz really (10Hz and 30 mj) because 3 Hz and 30 mj (.09watts ) is just to slow for my liking but my question , this low wattage of .09 watts or .3 watts will it be strong enough to kill bacteria. No one has done this study.
Does it cause the foramen to open up ( I am sure it will if you hold it down there for more than a second or two)
Its just a study I posted to show that there are alot of variables for success without widening the foramen or causing bleeding from the apex.
Time, energy, tip size, rate of movement all have an effect so we need a study that specifically assumes that the laser will work but at what settings.
THe Opus tip has a sealed end and a cheese grater openings that spiral along the side of it. The problem for me was that the tip was HUGE and not easy to get into canals except those that were massive.
I like the principle though of sealing of the end of the tip and getting a spiral type of effect. I dont think it would be as flexible as the tips we presently have without fracturing either with this concept but this is how effective it could be.
Traditional irrigation tips get NOWHERE near the end of the root , nor does the irrigant, but my associate who loves endo is writing about side irrigating tips that are so small that they can go to the end of a 30 prepared root.
I think that this might provide bleach to the end of the root and I would like to see the laser be able to do the same or similar without fear of apical enlargement.
Hope that makes sense.
Glenn
Lee AllenSpectatorGlenn,
Thanks for correcting my math. I figured it out today in traffic that I moved the decimal too far. Funny how the mind will think of something off subject when not even thinking consciously about it. That would give 8 seconds to acheive the 100mj in the study.
If the internal dentine (for you, the Candian spelling) is at all like the external root, then .25 Watts is just at etching level and not removal and should work.
I cannot imagine that any movement would have been called for in the study since it is too difficult to quantify.
Interesting thought about enlarging with the withdrawal technique starting away from the apex and when complete, going for full length at lowest energy stationary for 8 seconds to eradicate the last of the bioburden.
Now for the studies to verify. I will hold my breath.
Glenn on the roadSpectatorHi Lee: this is a great discussion and as you and I bounce things off I think I will start trying the two settings.
I will try and use something like 1 watt or so with the withdrawal technique and then at the apex use the lowest energies possible (between .09 watts to .30 watts).
I will check to see if one causes bleeding while another doesnt. What ideally I would like to do is find a setting that is just below the apical enlargment and use that . Bleeding is a good sign that the energy is to much so that is a good sign to look for. I can check the bleeding with either the small suction tips from Ultadent, or paper points.
I am off to the ALD and hopefully will be able to get some ideas on this topic.
Great posts Lee, I really enjoyed this discussion.
Glenn
-
AuthorPosts
