Forums › Other Topics › Consultation › Fractured Post/Core/Crown on Tooth#9
- This topic is empty.
-
AuthorPosts
-
SwpmnSpectator32 yo female presents with chief complaint of “loose crown” on tooth #9. She reports that the crown treatment is approximately 7 years old. No medical history concerns other than patient smokes tobacco. Radiograph and exam reveals endodontically treated tooth with dislodged post while the crown remains cemented to the core buildup. Tooth is fractured at the height of the gingiva.
Periodontal probing depths from crest of gingiva:
MesioFacial=2, StraightFacial=5, DistoFacial=3
MesioPalatal=2, StraightPalatal=2, DistoPalatal=3Occlusal exam reveals deep overbite with heavy occlusal wear on lingual of maxillary anteriors. All teeth show signs of occlusal trauma.
Please review photos/radiograph and offer treatment planning ideas to solve this patient’s dilemma(as well as my own):



[img]https://www.laserdentistryforum.com/attachments/upload/williamsa082404-4.JPG[/img]Thanks for your help,
Al
dkimmelSpectatorAllen, Looks like fun
I would first confirm there is no fracture on thhe facial.
– remove the crown palce a temp and new core.
– I would then do Cl on the max anteriors. It looks like your going to be lucky in that the CEJ of the centrals are in bone. Her smile is going to look better then before as she has a somewhat of a high lip line.
– a splint would be a good idea and ortho if she is up to it.
– If we are wishing — Grafting on the lower left would be nice.
David
Dan MelkerSpectatorHet Allen,
A case of Altered Eruption. Very common with traumatic injuries in young patients. I think I am right about previous injury as young adult. Should be quite simple if the post has done nothing terrible.
Treatment plan:
1. Retrieve post and place new post and core with provisional.
2. Gain visability to buccal of #9. Reshape root surface and remove excessive tissue but conservatively so as to have plenty of AG remaining. Look at #8 and remove bone as necessary to create space for BW if necessary. Place tissue at level of #8 for ideal symmetry. I will leave the procedure up to you as far as the use of the laser.
Thanks,
Danny
Be real careful with the frenum as it probably attachs near margin of MB of #9.(Edited by Dan Melker at 6:23 am on Aug. 25, 2004)
Dan MelkerSpectatorHi Allen,
hope you do not mind me posting. APE or AEE case makes it very simple if no fracture. Did not want to go into details.
Any questions let me know.
Should be an awesome case
Thanks,
Danny
After a close evaluation of the frenum the tissue should absolutely not be GV’ed away. The fenum is to close to the margin of tissue and could create a very severe problem if a GV is performed(Edited by Dan Melker at 9:10 am on Aug. 25, 2004)
SwpmnSpectatorDavid and Danny:
Provided I can determine there is no root fracture and based on what you have seen/info provided, you both feel that extraction and placement of a dental implant/crown complex is not indicated? Patient was not too thrilled when I presented this as an option. Big picture concerns are finances, patient is a fairly attractive young female in the public eye and I have to put one “right in the middle of the grill” on a lady with a high smile line. Psychologically she does not strike me as having unrealistic expectations.
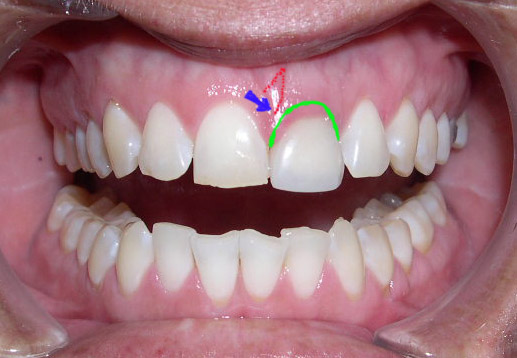
My eventual gingival tissue goal is outlined in GREEN. As Danny pointed out, it appears that the labial frenum attachment has erupted along with the dento-gingival complex toward the mesio-labial of tooth #9(marked with BLUE arrow). If I leave the frenum attachment alone, it will create an attached gingiva problem at the mesio-labial margin of the new crown(I feel sure there is also a biologic width problem here requiring some osseous reduction). My thoughts on the necessary frenectomy are outlined with RED dots.
Please review the photo and give me your opinion.
Thanks for your time,
Al
Dan MelkerSpectatorI would do a laser frenectomy first Allen. Then I would reflect a flap after about 6 weeks of healing. I would lightly reshape the flap on #9 and do any osseous necessary. You should try to match up the cej’s of 8 and 9 for symmetry. Place the tissue on #9 at the same height as #8. Then check to make sure you are comfortable with 6-11 before,cosmetically before you suture. I am sorry but I could not recommend Closed Flap Crown Lengthening
Thanks,
Danny
dkimmelSpectatorI could be wrong but I would think about bringing #8 up a bit. I think once you flap this the CEJ of #8 is darn close to the bone. You could easly bring the tissue up on #8 and then bring #9’s tissue up to match it. When you look at her over all smile, I think that would improve it.
How long is #8
David
Dan MelkerSpectatorAllen,
As I said in my post about looking at #8, my man Kimmel is right on. You can slightly Crown Lengthen #8 so that it will be more cosmetic related to #7. Obviously it would be ideal to make #8 and #9 a tad longer at the gingiva than #7 and #10.
Great point D. Kimmel!
Thanks,
Danny
Glenn van AsSpectatorI agree with Danny that it isnt a great case for circumferential closed flap crown lengthening.
Take an impression before you start, do a wax up for the temp.
Probe all areas for sulcus depth (oh you did) and then sound to bone to find out the BW. Make sure patient is anesthetized.
I would do the frenectomy first (probably with a diode to reduce the bleeding that is there)
I would try to remove the crown and check for fracture of the root ( A definite possiblity).
Now Unlike Danny what I might do is a GV on the Facial if that is where you need tooth structure if you want you temp to stay on without coming off all the time (ferrule).
I would remove enough gingival tissue to get 2-3 mm of tooth structure and then find out how much bone you had. I would do the GV with the diode laser to stop the bleeding. Make sure you dont go through the attached tissue. I would redo my prep at that time to get the ferrule effect. If you want make you temp.
Next off I would make a mini flap so as to get good visibility and remove the bone with the erbium at around 3 watts to 4 watts, first with a chisel tip or large footprint. Then finalize with a 400 micron tip.
You can mark the tissue that you want to do the GV with a sharpie. Mark the chisel tip with a sharpie to 3mm and remember that the 400 micron tip is around 2.5mm long (until it meets the teflon insulation, the quartz part is 2.5mm long…..convenient huh) and with the extra .5 mm for non contact you get your 3mm.
David Hornbrook taught me this as did Jack Miller from Hoya.
I would then suture and leave the temp in for a good 6 weeks and evaluate if you need to touch up the GV and see the healing of the tissue. Then take the impressions.
Not a great case for closed in my opinion, but then again what do I know!!
The laser can be substituted for the bur in this case, and remember to follow biologic prinicples of bone relief when using the laser (hows that Danny )
Glenn
Lee AllenSpectatorAl
I am curious what your patient decided to do in this case.
I have several variations of this case in my practice (sports injuries, mostly) and I just wanted to follow up on the outcome.Thanks.
-
AuthorPosts
