Forums › Laser Treatment Tips and Techniques › Soft Tissue Procedures › Guided Tissue Regeneration
- This topic is empty.
-
AuthorPosts
-
dkimmelSpectatorHave been reading Rossmann/Isreals article on Laser de-epithlializtion for enhanced guided tissue regenration. This seems real cool. They are talking about using a CO2 laser. So anyone doing this procedure? What are you using? Are you doing de-epithlialization prior to the flap as they sate or after the sx is closed?
I remember seeing a slide of this at the DT meeting in Vegas but most of that is a blurr now.
Thanks
DAvid
Robert Gregg DDSSpectatorHi David,
No need for flaps to de-epithelialize with pulsed Nd:YAGs and diodes. The perio and CO2 folks need to flap to gain access for their “free beam” lasers. It is really passe.
Check out the annimation on http://www.millenniumdental.com to see fiber-optically de-epithelialization at work with a pulsed Nd:YAG.
Bob
(Edited by Robert Gregg DDS at 9:48 am on Feb. 26, 2003)
Glenn van AsSpectatorBob Awesome animation very very neat.
Clap clap clap.
I like the web site and is this new or has it been there for a while.
Glen
PatricioSpectatorBob,
I enjoyed the animation. Can you share a little about the clinical progress one might expect to see in a typically responsive case of chronic periodontitis with loss of attachment and pockets exceeding 5 millimeters.
Over what time period and clinician time committment involved.
Pat
Robert Gregg DDSSpectatorWell thanks Glenn and Pat. Nice of you to kindly comment and glad you like it.
Glenn, the animation has been up on our website now for about a year.
The animation is something we give to our customers on a CD-ROM to use for patient education, or TV interviews, or lectures, or any personal use like that.
Pat! Have I got a case to show you….I just need to upload the photos for you. Give me a little while and I’ll have it done later today.
Thanks for the kind feedback!
Bob
Robert Gregg DDSSpectatorPat–
[img]https://www.laserdentistryforum.com/attachments/upload/Slide1.JPG[/img]
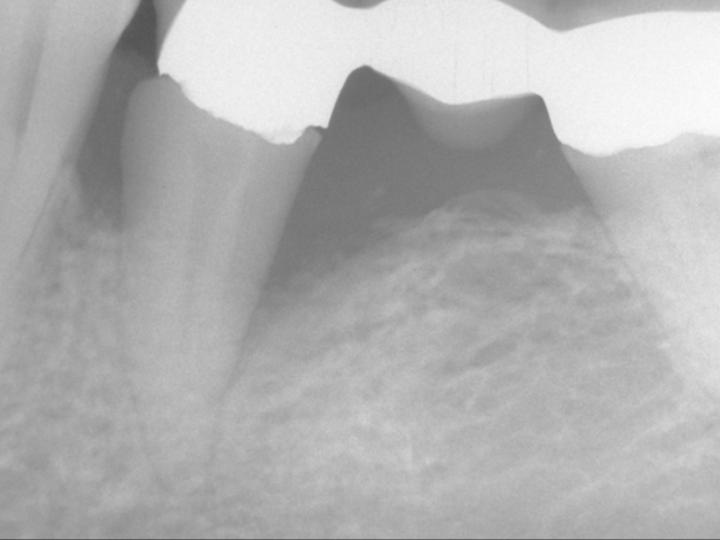
These pockets were 9-11mm deep on the facial. So greater than the 5mm you asked about.
[img]https://www.laserdentistryforum.com/attachments/upload/Slide2.JPG[/img]
This treatment was accomplished in December of 1997 with a PerioLase prototype FR pulsed Nd:YAG with variable pulse durations to obtain hemostasis and a “soft clot” w/o burning the tissue edges, carbonizing the tissue, creating epithelial peeling on the facial, or deep lateral thermal necrosis.
There is a “window” of optimal therapeutic energy and pulse duration parameters that is required to get this sort of result 4 minutes post-op. Diodes are just too hot and not able to control depth of penetration or surface heating of tissue the way a variable pulsed Nd:YAG can. It’s just he physics of different “waveforms” on and in tissue.
[img]https://www.laserdentistryforum.com/attachments/upload/Slide3.JPG[/img]
As this tissue continues to remodel, we can THEN decide what tissue refinements, recontouring, connective tissue grafting needs to be accomplished.
No probing will be done for 6 months. What reason to do so before then when the literature is clear that healing continues out 9-12 MONTHS post op? There was every expectation the hard and soft tissues would regenerate–and they did. Why wouldn’t they with this sort of 8 day post op result??
[img]https://www.laserdentistryforum.com/attachments/upload/Slide4.JPG[/img]
This patient was only treated once–and she was a heavy smoker
Hope you like it!
Bob
PatricioSpectatorBob,
This was a great visualization of this laser approach. I accept the visual evidence but would like to be assured that we are not looking at resolved gingivitis retaining the infection in the depths.What sort of pocket depth reduction would one typically expect and what typical final pocket depth vs normal 2-3mm? What is the long term reinfection potential and what is recomended for maintenance care? Finally, I would like purchase details for consideration. Thanks for all your help.
Pat
dkimmelSpectatorBob, Late getting back. The animation was great. I have referred by hygenist to the site as well.
David
Robert Gregg DDSSpectatorPat and David,
Thanks for your comments.
“I accept the visual evidence but would like to be assured that we are not looking at resolved gingivitis retaining the infection in the depths.”
Yep. Important to know. That’s why I usually show our radiographs, bone density studies and human histology, not clinical photos.
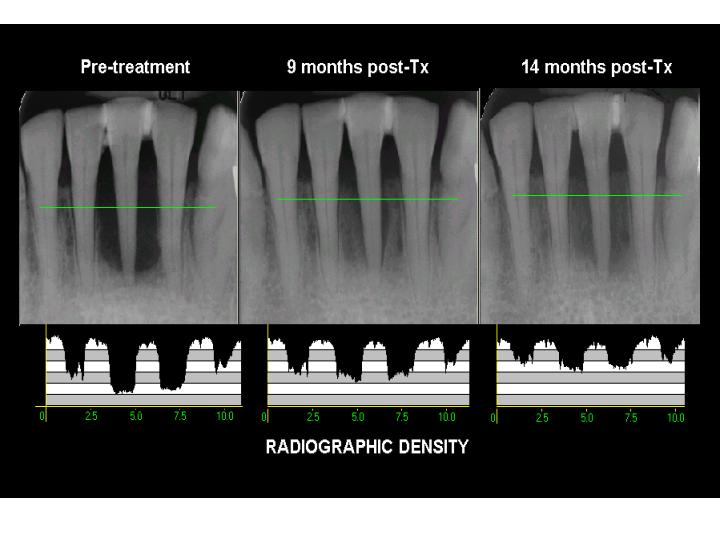
This radiographic series was subjected to bone density analysis using Emago digital comparative software to compare pixel to pixel in the radiographs compared. Bone density increased from 13% in the pre-op (through the section of film indicated by the green line) to 46% in the 14 month post op image for an increase bone density of 33%.

These are the clinical photos at 9 months. No probing was done before this appointment. Probes depths 2-3mm
“What sort of pocket depth reduction would one typically expect and what typical final pocket depth vs normal 2-3mm?”
blinded, multi-centered, retrospective, private practice clinical study
http://spie.org/scripts/abstract.pl?bibcode=2002SPIE%2e4610%2e%2e%2e49H&page=1&qs=spie
Study of 65 patients and over 1900 probing sites showed that laser periodontal therapy using a specific modality called “LANAP” for “Laser Ablation New Attachment Procedure” was reproducible in reducing 90% of pockets in ONE treatment by a minimum of 50% regardless of pocket depth as such:
> 4mm – 2.2mm reduction
> 6mm – 3.1mm reduction
> 8mm – 4.5mm reductionQUOTEWhat is the long term reinfection potential and what is recomended for maintenance care?Great question. Research over many studies and years shows that periodontal tissues treated using pulsed Nd:YAGs resist reinfection and breakdown longer by as much as 30 to 90 days over what SR/P alone can provide. But that is nothing you want to rely on with you patients who are ALWAYS suseptable to perio disease once they have it. So maintenance care is the same, 90 days, though many can be eventually pushed out at the discretion of the RDH.
QUOTEFinally, I would like purchase details for consideration.฼,995 all inclusive that includes the PerioLase MVP-7 digital pulsed Nd:YAG, 5 days of hands-on clinical training (includes 3 days of Laser BootCamp, extensive literature review), ADA-CERP/AGD-PACE CE’s, Jeff Mani’s laser reference, license for LPT, patented TrueFlex handpiece (nothing else like it), 6 months money back guarantee on getting clinical results such as those in the study above, hotel and transportation included (not air fare)–and for Laser Dentistry Forum participants–is an EMS Piezon 400 closed system ultrasonic scaler with the tips we use.
Thanks for asking and for your interest! Feel free to give me a call. If you want more info, I can mail you a packet of stuff with lots of before and afters. Just tell Laurie at MDT I said to send to a packet.
I’ll be at the Academy of Laser Dentistry Meeting (ALD) all next week–my first meeting travel since my torn Achilles tendon surgery last September….yeah.
Bob
MDT: 888-49-LASER
or 562-860-2908(Edited by Robert Gregg DDS at 10:39 am on Feb. 28, 2003)
PatricioSpectatorBob,
Needless to say this is an outstanding result. I will reflect on this option as I travel to South America beginning next week. We have a thriving and effective non surgical periodontal program and am always looking to improve it. I will call for the packet.
Pat
Robert GreggParticipantThanks Pat,
QUOTEI will reflect on this option as I travel to South America beginning next week.Ok………now just to tease you a bit more, reflect on this too while you’re gone down South. And if this doesn’t make you say “Uncle”, then I’ll have to post some more!;)
Have a great trip, and enjoy the warm weather!
Pre-Op x-ray of a vertically mobile bridge, that was treated with open flap, osseous surgery twice before presenting for treatment with LPT.
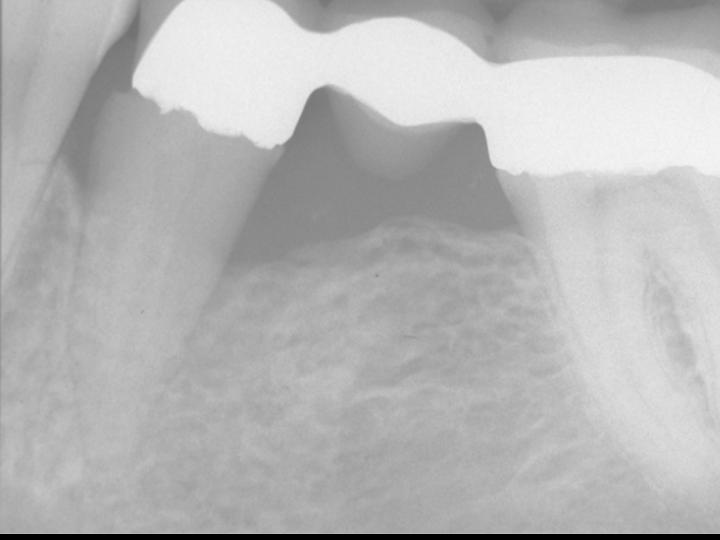
14 month post-op, after only ONE treatment with LPT/LANAP.
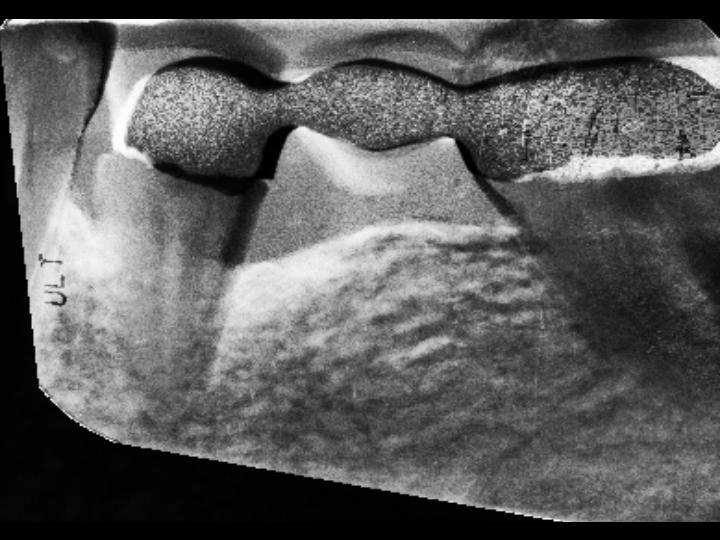
Gamma correction of the before and 14 month post-operative x-ray using Emago® software. White areas indicate increased bone density. Bone density increases extend circumferentially and 3-dimentionally into the alveolus.
Talk with you when you get back.
Bob
PatricioSpectatorBob,
Saw you pictures after my note on the weeping pulp. What can I say. This is outstanding. Anyone in the Michigan/Wisconsin area routinely using this process?
Pat
Robert Gregg DDSSpectatorThanks Pat,
Yes, Dr. Dick Holthaus, Janesville, WI.
But he told Del yesterday at the Chicago Mid-Winter, not to refer any more patients to him. He has all he wants to see!!
We get calls at MDT by patients looking for doctors trained by us. We refer them to our doctors around the country.
Other than that, no one else in your area.
But that might be a great opportunity for you. I know Dick wants to interect more with others using our protocol, yet he wouldn’t be in competition with you if you wanted to market the procedure.
And that’s a good point about marketing your lasers for anything, end result benefits–solutions for patients and what they are looking for.
Bob
-
AuthorPosts
