Forums › Laser Treatment Tips and Techniques › Soft Tissue Procedures › How to proceed?
- This topic is empty.
-
AuthorPosts
-
ELLIOT ROGOFFSpectatorNice Job Jetsfan, Maybe we should discuss the reason for rebound. If the biologic width is not invaded upon and we have 3 mm of sulcus why should their ever be rebound. Is the rebounding coming from not trimming the bone enough or at all and does this always happen. Maybe Dan could clear this biologic phenomenon up.It is not that we don’t want to do open flaps it is just that maybe we are not 100% sure of when to do them. Let’s get this topic cleared up once and for all.
jetsfanSpectatorGlen,
The patient is not in retention yet. Still active tx. The orthodontist just wanted the laterals to be proportional to centrals before he closed up the spaces.
Pre-op probing depths were 3mm on laterals and cuspids. Next patient , perhaps I will take photo of probing depth.
Immediate post op still had a 1mm sulcus. I will be curious to see what happens once brackets and wire are put back on. I do think there may be slight rebound on the mesial papilla of #10. At this point no surgery is required.
I used the Waterlase, with Rons topical . T-4 tip at .5W 11%A no water. Interesting enough, during procedure she felt nothing, but she did say it bothered her for a day or two after(not bad enough for tylenol).Robert.
(How about those JETS! …so far)
Glenn van AsSpectatorNeat Robert…….thanks for the added input.
My opinion is that unless the patient has those teeth extruded that there will be at least 50% rebound. That is what has happened to me in the past so as to let you know.
I think its great that you have done this but I have found that the tissue grows back unless we create the space. You can do it with closed flap but its not very precise or open flap.
I would think that the bone will come down with the teeth as you extrude them, but I would be interested to hear Dannys view.
Thanks for posting a neat case and I bet the patient is thrilled with the improvement and I do hope that it stays where it was put.
Thanks for clearing up the confusion on where the patient is with respect to treatment.
Glenn
Dan MelkerSpectatorHi Guys,
This is a case of Altered Active Eruption. The problem is that there is no space for the BW. In essence the CEJ is touching or approximating the bone. This case to be successfully treated must have a flap reflected to create a space for the BW.
You will see that the tissue will continue to relapse every 6 mths. There is no way to remove just tissue.
Take a good look at #8 and #9 they have major AEE.
I would not recommend treating this patient until she is 16 yrs. of age.
How can I be so certain, I did my share of trying to fool the BW unsuccessfully.
Thanks,
Danny
Notice the red collar of tissue surrounding the teeth that had crown lengthening. It will stay that way.
Finally, no further reshaping should be done because you do not want to remove any more attached tissue.
Thanks and have a great day!
One final point-notice the major discrepancy between #5 and #6 tells you the patient has generalized AEE. Finally, The reason for relapse is not the sulcus depth but the bone approximating the CEJ. Simply put there is no space for the BW. Until a space is created relapse continues to occur.
This is a great case to post because alot can be learned. I have been there!(Edited by Dan Melker at 8:34 pm on Sep. 28, 2004)
jetsfanSpectatorDan,
I agree this is a great learning case. I do appreciate your input. The dilemma was thus: laterals too small in relation to centrals.They needed to be bonded, but because of the eruption pattern, sizing these teeth was impossible. More tooth needed to be exposed. With 3mm of sulcus present , gingival recontouring was attempted. Teeth were bonded , achieving a good result. Will there be relapse? perhaps, IF so we will deal with it when she is a little older, but for now the ortho correction can be completed.
I look forward to your input on future cases that I post.Robert.
Dan MelkerSpectatorRobert,
I think the conservative approach you took for a 15 yr. old was a comfortable one. The long term situation is simply a need for further correction of the AEE-BW problem. There are times a nice conservative approach is appropriate and this is one. You will see that as this patient gets older the tissue on #8 and #9 will not move apically. The reason being is bone in the BW preventing apical migration.
An analogy would be if you have a 5 ounce glass and you put 8 ounces of water into it. The cup runneth over. No different here. There is simply no room for tissue so it will always runneth over.
Long term a huge difference can be made with osseous recontouring for a BW space. It would be recommended that no more GV’s should be performed because the tissue being removed is connective tissue that can well serve this patient.
Thanks for posting this case. It helps all of us.
Danny
Dan MelkerSpectatorAltered passive eruption and altered active eruption. In case 1 there is an adequate space for the BW when the tissue is reflected. If you wanted to use a laser to remove the tissue it would be successful.

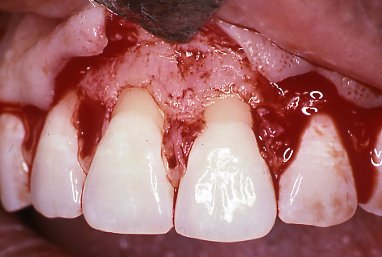
Case 2 when the tissue is reflected needs osseous recontouring to make a space for the BW. A laser can be used to contour bone but simply removing tissue will not work, relapse will occur.


Danny
kellyjblodgettdmdSpectatorDan – Nice pics to illustrate the significance of APE. This is a great thread.
Kelly
Glenn van AsSpectatorDan: EXCELLENT stuff……..this really helps. When you do remove bone, care must be taken with several things.
1. Size of tips (smaller tips create more vertical defects especially in the marrow spaces once you are through the cortical plate).
2. Settings should be medium to low in energy because again otherwise the cut is very rough and jagged.
3. Hand instruments are very useful for smoothing out.
4. It will take longer than the handpiece but you dont have much vibration or the sound of the drill with the laser.
5. Make sure water flow is high.
6. Angle the tip parallel to the tooth where possible to avoid iatrogenic notching of root surfaces and follow biologic principles of parabolic architecture so closed flap on these is not easy to avoid troughing if its a full anterior case.
7 Visibility is a must with a flap helping you particularly at the line angles and high mag is a great way to view carefully the interaction between the tip and the bone.
Rapid cutting is possible if you use to high an energy setting and you then will have a rough surface that hand instruments will be needed for.If the pockets measure 3-5 mm and you need a mm then perhaps gingivectomies will work, otherwise open flap for these bigger anterior cases is the way to go.
Glenn
-
AuthorPosts
