Forums › Laser Treatment Tips and Techniques › Hard Tissue Procedures › Laser apicectomy
- This topic is empty.
-
AuthorPosts
-
Graeme MilicichSpectatorThis was my first apicectomy. It was done on a very nervous patient who normally required IV sedation for conventional dentistry. I persuaded her to try this procedure without sedation, because I believed I could do it wothout having to use a drill or a scalpel. I booked her for 50 minutes. She was walking out of the surgery in 30 minutes!! I could not believe how wasy it was.
Initial incision T4 .75W 11%A 10%W. The flap was elevated using a periosteal elevator.

Initial access using a G6 Tip 2.5W 50% A 30%W. All the rest of the preparation including removal of the granulation tissue, amuptation of the root tip and cutting the apical retrograde cavity was done at this setting. No charring at any point in the procedure.
I have now reduced the air/water a bit more to help avoid the splattering that occurs at 50% A. (I needed to change scrubs after this first case, but it was fun and the patient was over the moon about how easy it was)


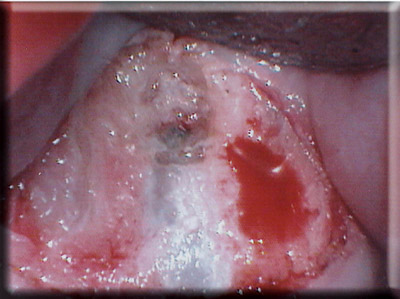

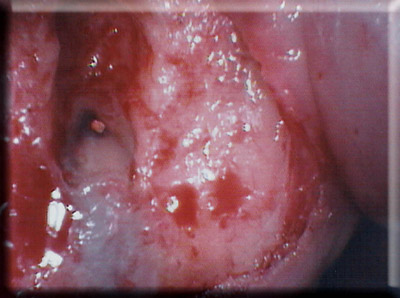

Accurate removal off the soft tissue was very easy with the Laser. You can still see some of the lobulated erosion of the bone that is visible in the initial PA.
As an aside, I have done several since this case and in two cases, ran into severe sparking when removing the GP for the retrograde cavity. I believe this is from cement like AH26 that has a very high silver content with the metal content of the cement causing sparking.
I just used a diamond tipped ultrasonic to remove the cement from the ccanal walls befoer finishing the prep.
Cheers
Cheers
ericbornsteinSpectatorDr Milicich:
Nice case. I have done many of these with my Opus Erbium lasers.
In my opinion, the sparking that you are seeing is probably more from the Zinc Oxide and/or Barium Sulfate impregnated in the GP cone (for radiopacity) than from the cement. Just make sure you have good evacuation and heavy water spray on the area being irradiated.
Eric Bornstein DMD
Robert Gregg DDSSpectatorVery nice case.
Local anesthetic? What type? Topical used?
Excellent photo quality, color balance and image clarity.
What camera set-up are you using.
I’ve been using a Global scope and a Nikon CoolPix 4500.
Thanks,
Bob
(Edited by Robert Gregg DDS at 9:39 am on Sep. 18, 2003)
marc andre gagnonSpectatorhi
I have done some cases like that and like you say it’s probably the type of cement that have been used whhich is the cause of that sparking
I have done like eric cases like that with erbium and with diode 980 and in all the cases we have very good results
excellent photos
thanks for sharing with us
SwpmnSpectatorExcellent. Did you close with sutures? Could laser “tissue welding” have been used, perhaps with a different wavelength?
Al
Graeme MilicichSpectatorQUOTEQuote: from ericbornstein on 8:07 pm on Sep. 18, 2003
Dr Milicich:Nice case. I have done many of these with my Opus Erbium lasers.
In my opinion, the sparking that you are seeing is probably more from the Zinc Oxide and/or Barium Sulfate impregnated in the GP cone (for radiopacity) than from the cement. Just make sure you have good evacuation and heavy water spray on the area being irradiated.
Eric Bornstein DMD
The sparking was only coming from the walls of the canal. The GP cut out without problem. On all the other cases, there has not been any problem with the GP, just on a couple of occasions with the cement
Cheers
Graeme MilicichSpectatorQUOTEQuote: from Robert Gregg DDS on 9:37 pm on Sep. 18, 2003
Very nice case.Local anesthetic? What type? Topical used?
Excellent photo quality, color balance and image clarity.
What camera set-up are you using.
I’ve been using a Global scope and a Nikon CoolPix 4500.
Thanks,
Bob
(Edited by Robert Gregg DDS at 9:39 am on Sep. 18, 2003)
LA was used. (Xylocaine) Patient was not one of those you would push the boudaries with!!
The photos were taken with a Reveal intraoral camera. I find I can get better views with it compared to the Microscope where I am often using a mirror. These tight areas are sometimes difficult to get a straight line view of with the scope and I find using mirrors slows you down too much. (The whole case including photography took 30 mins)
Cheers
Graeme MilicichSpectatorQUOTEQuote: from Swpmn on 4:17 am on Sep. 19, 2003
Excellent. Did you close with sutures? Could laser “tissue welding” have been used, perhaps with a different wavelength?Al
I closed with sutures. There was too much tension on the incision site to close with welding. I would only attempt to close with welding if the incision line is passive.
Cheers
Glenn van AsSpectatorNice case Graeme and nicely documented…..clap clap clap.
I will say that Dr. Gary Carr makes small mirrors that are super reflective, will get into these hard to reach areas, have necks that are bendable on them.
THey are marvelous……..
Great pics and thanks for sharing.
Glenn
PS I am gonna do one too one of these days but I wont try to break your 30 min mark.
Grin
glenn
Graeme MilicichSpectatorI have now got two month follow-up Xrays.
Here is the post op Xray and then the follow-up at 2 months.
I have to say I am impressed at the healing that has occured already.Cheers
(Edited by Graeme Milicich at 3:29 pm on Oct. 21, 2003)
SwpmnSpectatorMe too. Looks very nice Graeme.
Al
ASISpectatorVery nice case, Graeme.
What was the material for the retrograde fill? Not back bone fill in just 2 months.
Andrew
Graeme MilicichSpectatorRetrofill was MTA
The infill of bone amazes me. Tee Xray was taken 9.5 weeks after the initial one. I didn’t place anything in the site following the debridement.
Cheers
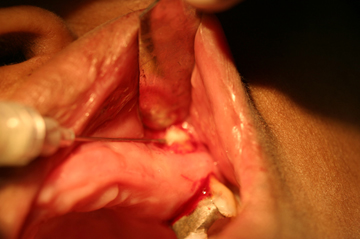
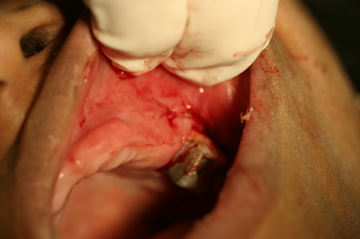
jetsfanSpectatorHere is my first max molar apico.
Patient had endo done and redone but pain persisted. Endodontist believed MB root probably sticking through buccal plate and needs apico. I told her I would do it with Waterlase. I used .5Carpule 2% lido 1:100,000epi.
outlined semilunar incision at .25W, then incised at .5W 11A 0W.
Flap elevated and sure enough there was the MB root. At 1.5W 15A 15W I enlarged the opening in bone, curetted granulation tissue, bevelled root and sterilized area. As patient has trouble taking oral meds I filled bone cavity with atridox, then sutured.
Patient did great, procedure was quick and post op was uneventful and her pain is gone.(I an not very good at posting photos. I hope the sequence is correct.)Robert.





Lee AllenSpectatorRobert,
Nice case and nicely done. I too have a Waterlase and have done only a couple but our technique is similar. I do use some water during incision only since I have done some non anesthetic skin tag removal on myself and find that it is HOT without some water. The heat must have some latent tissue effect. It does however have less bleeding without as your photos reveal. Nice posting of the photos, by the way.
I noticed that you did not use a retofill. Was it because your case was clean at the apex in comparison to Graeme’s case where the apex had a discoloration around the apical foramen perhaps indicating a leakage or intracanal chromatogenic bacterial saturation prior to the fill ?
Did your endodontist have some idea where the MB canal was so you could make the cut accordingly? I have done molar endo for 30 years and find those 4th canals end up in the strangest places sometimes. It would seem important to retorfill if found by apical cut. I wonder if you go success from cutting back to a place below the accessory canals? Who knows?
I have never tried the Atridox in the apical surgical site before but like the results you got. Is this your standard modus? Are there times when you would not place it?
Post Op pain is very difficult to manage since it comes from so many possible origins. You did well to erradicate it for your patient. Well done.
I just reread this message and realize that while I wanted to comment on the success but found that I have left you with many questions unintentionally. Sorry, but this helps me figure out how best I can use this for my patients with endo PO pain.
-
AuthorPosts
