Forums › Laser Treatment Tips and Techniques › Hard Tissue Procedures › Root Amputation
- This topic is empty.
-
AuthorPosts
-
ASISpectatorHi All,
This is a case of root resorption on the mesiobuccal of the right upper first molar that I have been trying to treat for a couple of years or more, but the patient was never ready. I am glad that he procrastinated as the erbium laser is definitely a better tool to provide the treatment with.
Pre-op
[img]https://www.laserdentistryforum.com/attachments/upload/johnH1dlf.JPG[/img]
Pre-op prior to endo treatment
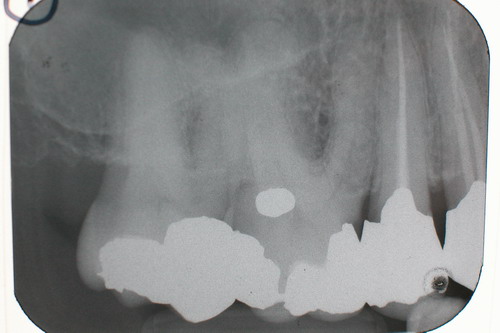
Pre-op after endo treatment

Pre-op showing resorption
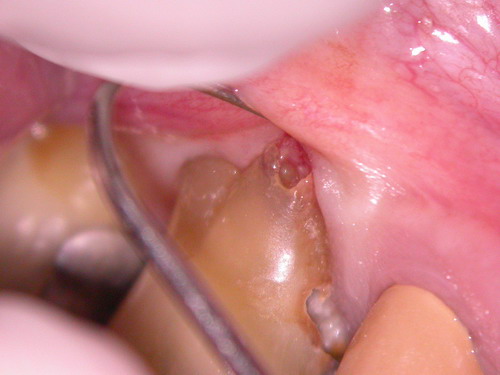
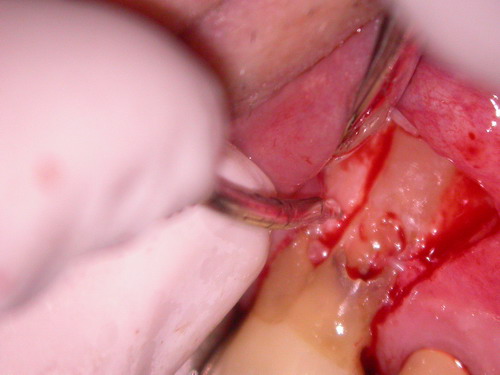
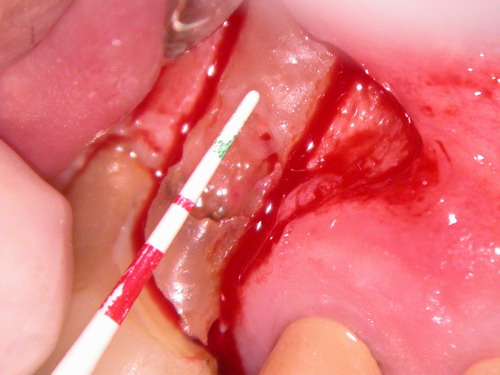
Er:YAG outlining incision @ 20Hz 35mJ dry
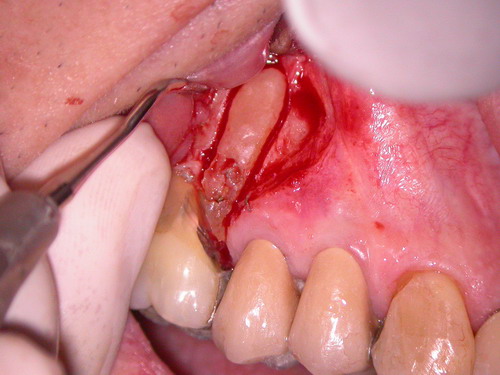
Flap raised

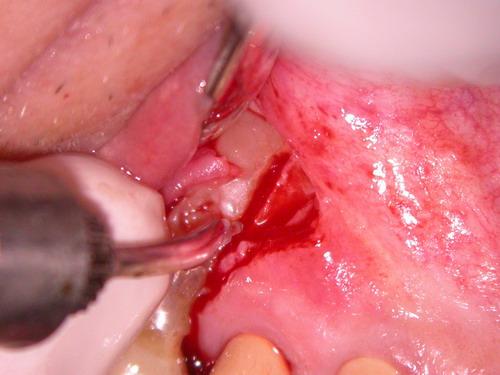
Full extent of resorption visible
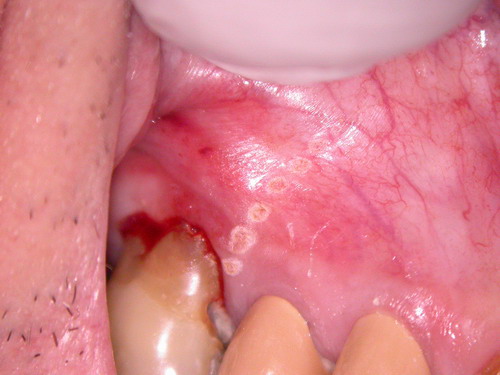
Troughing of distal aspect @30Hz 95mJ wet
Troughing of mesial aspect @30Hz 95mJ wet
Amputation @ 30Hz 160mJ wet
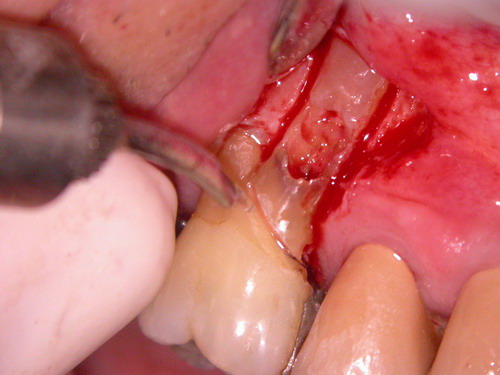
Amputation continued and finished by handpiece due to depth
5mm length to resorption
Troughed outlining of root but still ankylosed
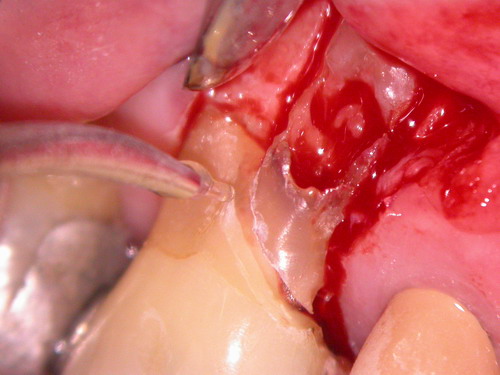
Root luxated prior to removal

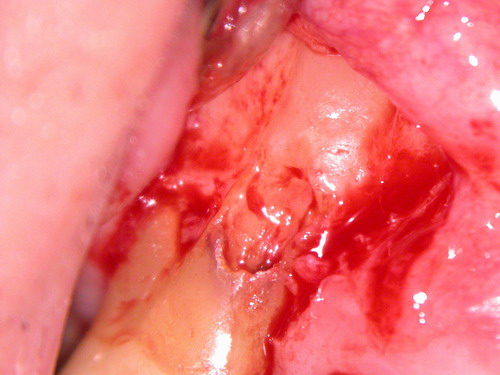
Root removed

Site smoothed with surgical chisel

Root with ankylosed bone fragments

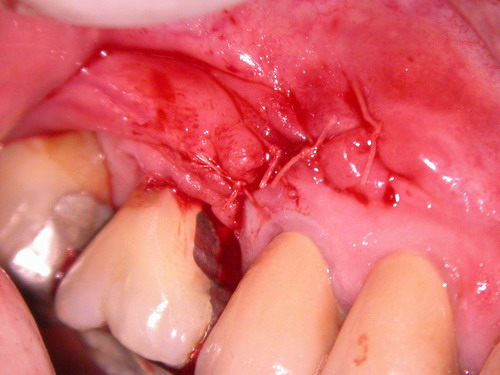
5-0 vicryl sutures placed
I’ll post a post-op radiograph at another time. Sorry for such a long post. We checked with patient and he’s had no real discomfort aside from mild soreness in area. I don’t think he would fare as well without the use of the erbium wavelenght.
Cheers,
Andrew
Glenn van AsSpectatorReally cool pics Andrew and the visibility with the erbium when cutting bone is really great as the water spray cleans the surface but doesnt splatter. Very little ablation products as well.
I have videotaped one case like this as well and it was an upper molar and the MB root which was vertically fractured. Mine was a little easier to get out due to its length.
Neatly handled and thanks for the great post.
Glenn
kellyjblodgettdmdSpectatorAndrew – what a cool post! Very well documented. Isn’t it beautiful how little post-op discomfort patients have with these treatments?
Just a question – Was restoring the root with Geristore an option? I’ve read that PDL fibers can re-attach to the material. Or maybe some MTA? Just curious.
Kelly
ASISpectatorHi Glenn & Kelly,
Thanks for the feedback.
Restorative treatment is certainly an option but with the extent of resorption and even if successful endo was done to the MB root, it will be a highly questionable structurally. In the meantime, the presence of root decay on the mesial aspect was not helpful and certainly dealt with by the amputation.
Thanks.
Andrew
kellyjblodgettdmdSpectatorI think I would have done the same thing, but I’m sure it wouldn’t have been so pretty. Nice pics.
Kelly
drcamSpectatorI’m with Kelly I feel this lesion could have been successfully treated with rct, trichloroacetic acid and either geristore or glass ionomer. The great difficulty long term with root resection long term is cleaning them. eventually they tend to rot out underneath. Good use of the laser though with the treatment option you chose.
Cheers Cam
Glenn van AsSpectatorHaving done root resorptions before , this one was huge and in combined with the root cariies it would have been very difficult to save.
I think that the treatment provided here was very good alternative to the TCA and Geristore.
Remember that to treat this case without a scope is suicide…….
Nice stuff Andrew.
Glenn
Robert Gregg DDSSpectatorVery nice case Andrew. The long term prognosis is better than RCT, MTA from my experience and in my hands. Especially as Glenn pointws out about the size and the caries. That’s just a lot of things working against a good long term results.
Well done, I like you use of the laser for this, the microscope and your photo-documentation.
I would allow this case as one for your advanced proficiency!!
Bob
Bob
ASISpectatorHi Glenn & Bob & Cam,
Thanks for the kind feedback. I had a chance to present this case a couple of weeks ago with Dr Michael Swick when he was doing a two-day Standard Proficiency course in Vancouver with The Institue for Laser Dentistry.
I hear what you are saying, Cam. I’ve had cases when poor plaque control compromised the longevity of an amputated treatment. In this situation, it may be the more predictable way to go. The patient is on home fluoride use with custom trays by the way. At least, he knows he is supposed to anyway.
Cheers.
Andrew
lookin4tSpectatorHmmm…my post got lost.
Glenn, there are a ton of guys not using a scope that this works for in the high 90s as far as % over 10 years with proper case selection (Fugazotto for one). I don’t think it is suicide without a scope.
Next, does anyone give any thought to grafting the socket at the time of removal? This is a self-contained defect for a graft now..that will be more difficult to fix later. There are some long term studies on root amps that don’t paint a rosy picture…..any thoughts on setting this up in case it ends up an implant later?
-
AuthorPosts
