Forums › Laser Treatment Tips and Techniques › Soft Tissue Procedures › Short versus Long Pulse Comparison
- This topic is empty.
-
AuthorPosts
-
Robert GreggParticipantHi Everybody,
Here’s a case I had to deal with today on an uxpected basis. Patient had a C/C of sore gums. At first I used air and vacuum (to cool and for comfort) Fr Nd:YAG at 3.00 watts, 20 Hz and 100 usec pulse duration without local anesthetic.
[img]https://www.laserdentistryforum.com/attachments/upload/Eva1.JPG[/img]
After giving Lidocaine 2% with Epi 1:50,000 I tried again at a higher wattage but same PD of 100 usec. No such luck in getting hemostasis.
[img]https://www.laserdentistryforum.com/attachments/upload/Eva2.JPG[/img]
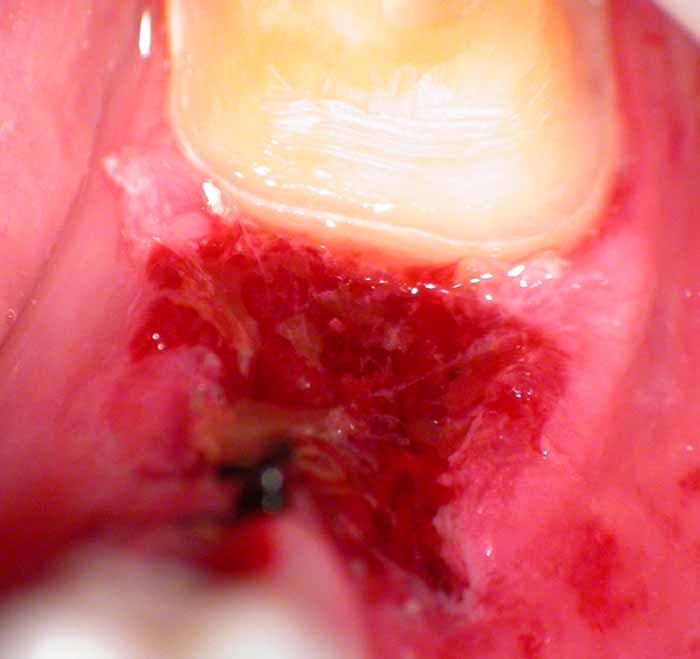
After anesthesia, I used a long pulse duration setting of 650 microseconds. Since I had disrupted the tissue and capillary vessels (opening them up), it took a little more effort and energy to get the area to calm down.

This is the kind of control over the tissue and bleeding that is possible when one can vary the pulse duration of a near infrared pulsed laser. Note the lack of char, zone of coagulation, or epithelial peeling. No post op recession for this patient………
[img]https://www.laserdentistryforum.com/attachments/upload/Eva4.JPG[/img]
Starting off using a longer pulse duration on hemorrhagic tissues avoids disrupting the tissue and
vessels with high peak powers of short PD (1500 watts per pulse), and getting immediate hemostasis, thus saving time & less irradiation exposure to tissue, i.e. proper “Light Dose”. Less chance of thermal injury to tissue that way through economy of energy.May 22, 2003

This is the missing Pre-Op x-ray showing the defective restoration.
This is the 7 day post-op. NOTE: Any recession or loss of tissue height?
Bob
(Edited by Robert Gregg at 4:38 pm on May 22, 2003)
Glenn van AsSpectatorCool case Bob and very interesting to see how pulse duration can affect hemostasis……I learn something everyday.
Can the long pulse duration also be done without anesthetic.
Was there a difference in pain perceived between the two sides.
Glenn
Robert Gregg DDSSpectatorThanks Glenn,
You can use long pulse durations w/o anesthetic if you are careful. Especially when you can select 250, 350, 450, 550 and not be limited to only 650 as your long pulse setting.
More exposure time = more chance for pain. And the exposure of 650 is 6.5 times longer than the very short 100 microseconds PD.
But most of the time, when the tissue is this messed up, it’s time to numb and get the job done, which is what I did.
Bob
SwpmnSpectatorSo………here’s my question:
Is the ability to obtain hemostasis more a function of wavelength or of pulse duration? Doesn’t a wider pulse duration invoke a wider band of thermal necrosis and thus achieve the desired hemostasis?
If I could vary and thus increase the pulse duration on my Erbium from say 150 to 550 microseconds would I see an improvement in hemostasis in soft tissue? How come today’s Erbiums don’t come with user adjustable pulse durations? I guess the Cavilase that Jack Miller showed me one time did have a variable PD – anyone know if the PD is “user-selectable” on the Opus Er:YAG?
Al
Robert GreggParticipantHi Al,
I love how you are thinking about this!!
“Is the ability to obtain hemostasis more a function of wavelength or of pulse duration?”
More of pulse duration.
Doesn’t a wider pulse duration invoke a wider band of thermal necrosis and thus achieve the desired hemostasis?
I’m impressed with your analysis. Not quite, but that’s pretty close. With conditioned or initiated fiber tips, yes. With unconditioned pulsed laser fibers with high peak powers, no.
Thermal (coagulation) necrosis is a surface effect of laser wounds. Varying the pulse duration will effect the deeper layers below the surface zone of coagulation/necrosis—the zone of injury or stasis.
A wider pulse duration gives a wider zone of thermal injury or “stasis” i.e. hemostasis—not necessarily a wider surface zone of coagulation or thermal necrosis – unless it is a short pulse duration of a deep penetrating wavelength (1.064).
That’s why being able to VARY the pulse duration we can vary the effects from a surface effect only, or a gradually deeper effect on the zone of stasis to get HEMOSTASIS without necrosing the surface. That’s why the pictures look so un-effected on their surface. They are! And that’s how we are able to get the wet “soft clot” not the dry necrotic wound (eschar) you would see with an initiated contact fiber laser.
Does that make any sense?
Here’s a photo I took today of a stable fibrin clot in an extraction site after I removed the tooth and lased the site at 4.0 watts, 20 Hz, 150 usec for 200 Joules with a 360 micron fiber. The patient is taking 100mg of aspirin a day and says he tends to bleed easily. Ha! Not around me he won’t. This distal tooth was prepped after getting the clot so I could watch the clot stabilize. It stabilized in about 3 minutes and only got more stable as I prepped the tooth. This is the photo after I prepped the tooth – 10 minutes later. Ready to make a temporary. That black thing there is a suture. Contrary to my periodontist friends, I do use a blade and sutures once in a while (root decayed below the gums)
Here’s a general description of laser wounds from the surface down:
Histology of the Laser Wound
1. zone of ablation – the zone of vaporized tissue (or not)
2. zone of coagulation (necrosis) – the surface of the wound.
3. zone of stasis (injury) – deeper and peripheral effected zone
4. zone of hyperemia (edema) – deepest tissue zoneFurther defined:
ZONE OF COAGULATION (NECROSIS)
This zone is comprised of the surface tissue necrosis of the initial burn eschar. Irreversible injury.ZONE OF INJURY (STASIS)
Deeper and peripheral to the zone of coagulation, there is an area of tissue injury where cells are viable but can easily be further damaged. Fibrin deposition, vasoconstriction, and thrombosis occur. Early epithelial cell death in this area, unrelated to blood flow, can be quite high, leading to slowing of healing.ZONE OF HYPEREMIA (EDEMA)
Peripheral to and below the zone of stasis is the zone of hyperemia. The area is characterized by minimal cell injury but with vasodilatation (edema) due to neighboring inflammation-induced mediators. Completed recovery of this tissue is expected unless there is an additional severe insult such as an invasive infection or profound tissue inflammation.QUOTEIf I could vary and thus increase the pulse duration on my Erbium from say 150 to 550 microseconds would I see an improvement in hemostasis in soft tissue?Unfortunately, no. It’s due to the fact that erbium being highly absorbed in any tissues in the mouth, you would not get a deeper effect on the zone of stasis, but a deeper effect in your zone of ablation and the amount of tissue vaporized.
QUOTEHow come today’s Erbiums don’t come with user adjustable pulse durations? I guess the Cavilase that Jack Miller showed me one time did have a variable PD – anyone know if the PD is “user-selectable” on the Opus Er:YAG?Erbiums are still evolving. The devices on the market today are 2nd and 3rd generation. Cavilase was going to be about 4th generation erbium with its 3 different pulse durations (100, 250, 350 or something like that). The PerioLase 5th generation. But the erbiums are ALL still analog versus digital for the PerioLase, which makes selectable pulse durations so much easier and efficient. The technology for the erbium is still developing compared to the technology for the pulsed Nd:YAG to some extent.
Also, the manufacturers will need to understand that there is a clinical need for different PDs. For that to occur, the clinicians need to be able to determine (as Del and I did) how different pulse duration effect, in the case of erbiums now, hard tissue differently. In some respects, we have a means to compare two different erbium pulse durations – Waterlase at 90 to 140 microseconds (depending on who’s numbers you accept) and DELight at 240. That’s a significant spread. I think that while very similar, there are advantages at times to using the 140 usec say over the 240, and vice-versa. Now combine that difference in pulse duration and add the effects of different rep rates and higher millijoules per pulse, and now even I am getting interested in the erbium. (Oh, that’s right, I’ve ALREADY been interested since 1990……..).
So quite literally, the advances in erbium devices will be the direct results of clinicians like Glenn, Bryan Pope, Mark Colona, and others who pay careful attention to the effects of different parameters, and engineers listening to what the clinicians are saying (a very hard thing to occur), and THEN do something about it. But the clinicians are KEY to the next big advance in erbiums. Like we talked about at CDA Anaheim.;)
Great questions!! Thanks for asking. I love it when I have to stretch my mind to make sure it makes sense on paper.
Bob
Glenn van AsSpectatorHEy before I read the rest of the post……….COOL photo.
Nice picture, now you are getting the hang of it. It took me forever to take the pictures and get them that good…..I hate to see where you will be in another 3 months with the scope , digital camera etc…….
GRIN
Nice stuff.
Glenn
Robert Gregg DDSSpectatorThanks Glenn,
I AM getting the hang of it! And I owe it ALL to you!!
My first pics (as you saw) were for s _ _ t.
I’m really only as good as you have helped me to be!
I LOVE being coached by a skilled Master and excellent teacher, as you are. The student is the reflection of the teacher, don’t you think?
You are my photo Yoda!:biggrin:
This is just an incredible way to communicate clinical dentistry and the effects of technology. Unfortunately, it is such a powerful medium it can cause some negative reactions, as well as positive impressons.
Can I borrow your flame retardant suit next time I post on Dental Town? Ha!
Bob
Robert GreggParticipantSee above editions/additions.
-
AuthorPosts
