Forums › Laser Resources › Laser Physics Related Literature › spreadsheet comparing thermal damage from experiments
- This topic is empty.
-
AuthorPosts
-
lagunabbSpectatorI made a table comparing thermal damage zone results and settings from the Wang et al (2002) bovine bone experiments and the Eversole et al (1995) experiments on rabbits and beagle dogs. It is in Excel format and tab-delimited txt format at
txt file: (can be read into older versions of Excel)
excel” target=”_blank”>http://etechadvisors.com/PDF/thermal-damage_comparisons.txtexcel file:
Please” target=”_blank”>http://etechadvisors.com/PDF/thermal-damage_comparisons.xlsPlease feel free to download it. Comments are welcomed. If you have other hard tissue experimental data to add (all wavelengths) send me the paper or send me the new spreadsheet if you decide to add it yourself. Thanks.
Glenn van AsSpectatorHey Ray……had a look at the excel sheet……cool.
One thing i noticed is that the water was 20ml/min.
Now Ron Schalter was mentioning that there was a study showing 1.62 ml / min as being the most efficient for ablation with a erbium yag only laser.
I measured my output and found I was at 9 ml / min so I lowered it.
SOme have mentioned that 20 ml / min is around 20% depending on the air ration (20-30 ml)
What is interesting is to see the large changes in water flow between Biolase and others in the Er Yag family.
I wonder if this is just coincidental or is there a logical reason for why the Er:Cr: YSGG requires more water. The simple answer would be that HK requires it, another might be that heat generation is greater with Biolase.
I dont know the answer and believe me am not looking to stir things up but Allen Williams mentioned to me personally that it was one of the things he notice first was the difference in water flow between the two lasers and I felt bad about my 9 ml / min til I started ready others using 2-3X what I am.
I really like the spreadsheet and saved it for the erbium chapter.
I bet that in 5 years there will be a wealth of material out there on all sorts of things with respect to lasers that arent out now.
I have often said that I always took it for granted that the laser improved bond strength ( regardless of brand) but now I really wonder about that because alot of the research doesnt support that.
One thing clinically that I always notice is that there is a big difference after I finish with the laser and I etch with phosphoric acid and dry in the dentin surface……(see my picture below) and I know that the laser has already removed the smear layer and opened the tubules so what is the etch doing to the dentin…….
Removing ablated material??
I just wonder?
ANyways thanks for the studies…….good stuff and again by way of public disclosure this post is not meant to inform anyone that any laser is superior to another by the statements I have made.
Glenn
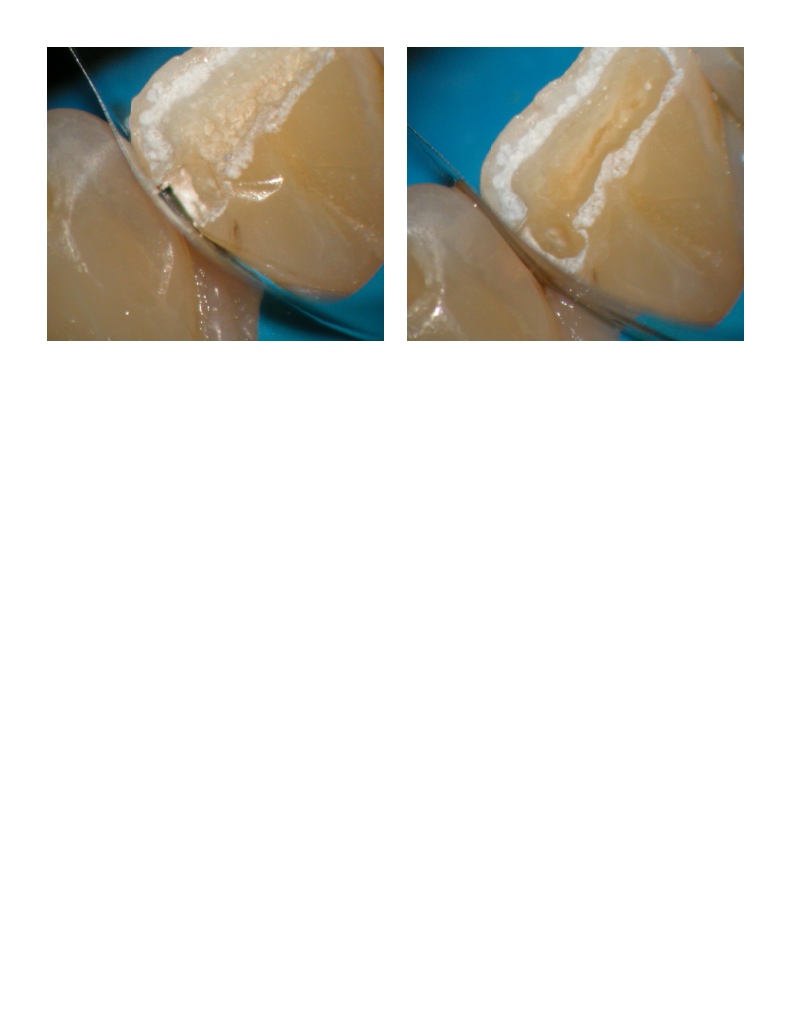
Glenn van AsSpectatorOops…..here is the image.
Only differenc is image on the left is after laser preparation completed and on the right is after acid etch for 20 secs.
Why did the dentin change color?
Glenn
lagunabbSpectatorGlenn,
“I dont know the answer”same here and glad you found the table informative. My understanding of the DElight water delivery method is that it is more direct so it may be that you don’t need as much volume compared to the sprinkler style dilivery of the Waterlase. I also think there may be some subtle differences because the DELight tip is kept closer to the target tissue (0.5 – 1 mm??) so it is essentially a water film versus droplets + water film in the case of the Waterlase which is kept 1 – 2 mm from the target tissue. Both approaches seem to work fine.
AnonymousGuestQUOTEQuote: from lagunabb on 3:01 pm on Oct. 31, 2003
Glenn,
“I dont know the answer”same here and glad you found the table informative. My understanding of the DElight water delivery method is that it is more direct so it may be that you don’t need as much volume compared to the sprinkler style dilivery of the Waterlase. I also think there may be some subtle differences because the DELight tip is kept closer to the target tissue (0.5 – 1 mm??) so it is essentially a water film versus droplets + water film in the case of the Waterlase which is kept 1 – 2 mm from the target tissue. Both approaches seem to work fine.
Glenn, possibly the acid/rinse has removed the debris from the ablation?
Ray, wouldn’t the positioning of the tip be more of a function of focal length than where the water is?
lagunabbSpectatorRon,
” Ray, wouldn’t the positioning of the tip be more of a function of focal length than where the water is?”I am not sure. For the non-contact mode, I am thinking that both the focal length and water geometry/distribution geometry are equally important whether one assumes that water enhances ablation or if one assumes that it is mostly vaporization-cooling. ie you want to keep the spot size small enough to do the job for the power setting.
Glenn van AsSpectatorRon : My current thinking is that you are absolutely right in that the ablation by products are opening up the smear layer but that the debris is in the dentin. I dont think that rinsing off without etch will remove the ablation biproducts on the dentin without the rinse………..
soooo……clinically I wonder if the acid etch and rinse are needed not to open the smear layer but to remove the debris for best bonding.
THats what I do…….
If this is the case , will one of the lighter etches available do the same thing……
So many questions, so few answers but I agree with you that etch and rinse is removing the ablation material on the dentin in particular and gives us super open tubules. I do think only a 10 second etch might be enough with the laser already having etch the enamel and opening up tubules on the dentin that the etch is for removing debris, thats how I am using it now.
How about the rest of you………great ideas.
Glenn
AnonymousGuestQUOTEQuote: from lagunabb on 2:30 am on Nov. 1, 2003whether one assumes that water enhances ablation or if one assumes that it is mostly vaporization-cooling.
Amazing how often we return to that same question (no disrespect intended, Ray) and how it effects what we do or therorize about other laser principles. It still amazes me how many people want to blow off the answer to that question as being unimportant because all they care about is ‘it works’.
2thlaserSpectatorDo you guys think that the ablation debris, even though it’s disinfected by the lasers energy, is a type of “smear” layer, that needs to be removed, as Glenn and I do (Glenn mentions it above in his post, I do the same as he does with etch/resin)..?
Mark
lagunabbSpectatorRon,
“Amazing how often we return to that same question (no disrespect intended, Ray) “
Don’t worry about it. We are all trying to understand the science better and I agree that it is important for users to try to understand it as well. I get the impression that there have been many bonding experiments. There may be enough to make a nice big table comparing all the experiments. Any takers?
RE the Fried et al bonding paper:
I haven’t kept up with the latest experiments from UCSF and it is interesting to see Fried et al continued his water-augmentation experiments to address clinically significant issues such as bonding. Seeing that abstract makes me a little bit more comfortable about my interpretation that his 2002 water-augmentation experimental results showed a multiple higher ablation rate than can be explained by vaporization-cooling.(Edited by lagunabb at 9:15 pm on Nov. 2, 2003)
lagunabbSpectatormore thoughts about the bonding experiments:
The Fried et al experiments used clamps and holders for laser and target. This may also be the case in other published experiments. However, hands tremble and patients move so the experimental results has to be qualified in relation to real situations where the tip distance to the target may vary far from optimal. Depending on how shaky the dentist’s hand is and the patient’s head movement, you can go from “contact” with melted debris in crater to the Fried stated optimum of ~1 mm thick water layer and no smear layer.
(Edited by lagunabb at 8:15 am on Nov. 3, 2003)
SwpmnSpectatorQUOTEThe Fried et al experiments used clamps and holders for laser and target. This may also be the case in other published experiments. However, hands tremble and patients move so the experimental results has to be qualified in relation to real situations where the tip distance to the target may vary far from optimal. Depending on how shaky the dentist’s hand is and the patient’s head movement, you can go from “contact” with melted debris in crater to the Fried stated optimum of ~1 mm thick water layer and no smear layer.Ray:
From a purely clinical point of view I can tell you:
1) At 42, my hands are still very steady and I use definitive finger rests on adjacent teeth to insure accurate placement of the erbium laser tip.
2) The patient’s head is not moving. If there is any question of patient head movement due to apprehension or pain perception, I use local anesthetic.
3) My erbium laser tips are carefully used at a defocused 0.5 to 1.5 mm distance. 4.5X custom made operating loupes are combined with a directly focused headlamp to obtain an accurate, defocused application. The tips are not banging into the tooth and then swinging out to a 1.5 to 2.0 mm distance. Opus advocates a contact mode with the erbium which I still don’t understand. Contact with the Waterlase sapphires or DELight quartzs can result in damage to the tips and magnification may be the key. Since increasing my magnification from 2.5X to 4.5X now have tips from both companies which I have used for months with no detected decrease in ablation efficiency.
Al
Glenn van AsSpectatorInteresting post to show how magnification can really help not only with the length of time tips last but the ablation rate.
Lasers are a visually driven technology, as there is no tactile feel. Lots of water spray and a clear tip…..tough to see how close the tip is to the tooth.
You know what I am gonna do is tomorrow take a video of the laser at 2.5X power and one at 10 and 16X power to show how much easier it is to prep. I bet I could cut a deep trough faster at the same energy with 16X power than I could at 2.5X power…….If you can control the tip at the optimum ablation point regardless of which laser it is, you will cut faster.
Its a no brainer……..if you arent using loupes……get some.
Enough said……great post Allen
Glenn
Ask Kelly in 3 weeks what he thinks of scopes……..my guess is he wont stop talking about them…..I know that is how Mark feels as I talked to him about it at the CDA and he was using 6.0 power loupes.
Glenn
-
AuthorPosts
