Forums › Laser Treatment Tips and Techniques › Soft Tissue Procedures › Two Laser Frenectomy Cases
- This topic is empty.
-
AuthorPosts
-
BenchwmerSpectatorFollowing are two frenectom cases. The patients were both 24-25 year old white females.
For the first case the OpusDuo Erbium was used. An 800 micron conical contact saphire tip was used, delivered by a wave guide. Settings were 500mJ, 12 Hz w/ water spray (2.0W measured with a PowerMeter)
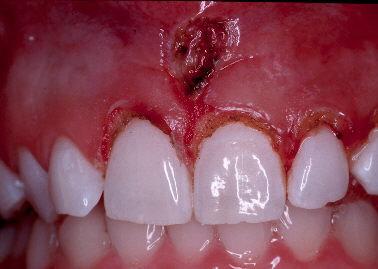
BeforeLA used, a couple drops of Carbocaine infiltration. The frenum was removed using a contact tip, pressure was applied to the tissue by pulling on the tissue w/ a tissue forcep. Exposure time was less than 10 seconds. Bleeding was stopped applying pressure w/ a damp cotton roll.

Photo immediately after treatment.

Post-op at seven days.
The next case was done with the PerioLase free running. pulsed Nd:YAG w/ a 360 micron contact fiber.
Settings 3.0W 20Hz 150usec. No water or air coolant.
Before photo.
Similar technique in LA, cutting the tissue under tension, no bleeding. Exposure under 30 seconds.
Immediately post-op. Also gingivectomies and tissue plasty were performed.

Post-op at 10 days.

Post-op at 4 weeks.
Comparing the two surgical sites at one week post-surgery. Shows little difference in healing. Neither patient needed any pain meds. Had no post-op complications.


I prefer the Nd:YAG for frenectomies, no bleeding, a slower, more controlled tissue cut. However, both lasers allowed me to use the same basic techniques, with the same results.
If I would of used the Erbium for the GVs, I would have had to alter my technique. To remove gingival tissue w/ the Nd:YAG, I am able to direct the fiber at a 90 degree angle to the tooth. The tooth is able to disipate the energy w/ no damage. Note how the tissue was scalloped. The Erbium would have to be used parallel to the tooth or damage would result. The Erbium uses a different technique, cutting faster and w/ bleeding.Jeff
(Edited by Benchwmer at 10:08 pm on Mar. 13, 2004)
mickey franklSpectatorThanks for sharing this great example.
Glenn van AsSpectatorHey Jeff: excellent example of how the erbium cutting of tissue for gingivectomy would differ in angulation of tip compared to soft tissue lasers. Great Point.
Nice photos and thanks for sharing.
Interesting that with the Erbium hollow waveguide that what starts out as 6 watts (500 mj 12Hz) ends up as 2 watts.
Now is this loss because of bending the hollow wave guide or is there some other issue I am not aware of.
Do you think it happens similarly with restorations. What settings would you use for occlusal enamel.
In closing I got a chance to cut with the Opus at the ALD and enjoyed it and learned some things that I like and a few I dont. All in all it was very enjoyable to see how the Opus cut under the scope and I thank Rick for helping bring the laser into the meeting.
Thanks in advance and nice photos of two great frenectomies…….thanks for posting.
Glenn
BenchwmerSpectatorGlenn,
The hollow wave guide I was told loses half power. The rest, mirror on handpiece, tip, bending the waceguide. Do you use a PowerMeter to measure tip output? Does anyone on Erbiums. I always test fire Nd:YAG on the meter.
Enamel 700mJ 12 Hz
Jeff
Dan MelkerSpectatorAs a Periodontist learning about lasers I still look at tissue. In the case with the mand. frenectomy I would suggest doing a soft tissue graft on #24. Removing the frenum will not correct the gingival problem.
As far as the GV on the centrals and lateral I think BW considerations should have taken place. To create a long lasting result I think osseous recontouring would be necessary.
Again, I know this is a laser forum and hope that these comments are not taken the wrong way. Treating the patient with a laser is great though I think we should still keep biologic principles in mind.
Thanks,
Danny(Edited by Dan Melker at 9:19 am on April 25, 2004)
BenchwmerSpectatorDan,
Your comments and proposed treatment mimic what I have always heard from my Periodontal community and was the reason I became a laser dentist five years ago, after 20 years practicing general dentistry.
I got tired of my patients that I refered to my local Periodontists being overmanaged and overtreated. Patients returning with exposed roots surfaces, root sensitivity, loss of papillas, black triangles and stories of the discomfort of scalpel/suture/packing perio surgery.
I knew there had to be alternative treatment modalities.
I found that they are out there if you look and learn.
The cases you commented on were shown to show the tissue response differences in using the Nd:YAY vs. Erb:YAG for frenectomies.
The complete case for the Maxillary frenectomy/GV case is under Nd:YAG procedures in this forum. Bilogic width issues were addressed. Probing , sounding to the crest of bone, radiographs etc were used. This case only exposed enamel, why would flaps, bone removal even be an option.
In the Mandibular frenectomy, a graft may be needed in the future, but there is a band of attached tissue, why even consider a graft now in this perfectly healthy, well maintained mouth?
What would you do if it was your mouth?
There are different treatments you and I can use to get the same results. Lasers allows me a conservative option to practice dentistry.Jeff
Glenn van AsSpectatorNice post Jeff and nicely done case.
glenn
AnonymousGuestDanny,
In the case w/ the mand. frenectomy, it appears to me that besides the frenum pull that occlusion and tooth prominence have also played a role. In your opinion, if the occlusion is addressed and the patient advised not to beat this area up with brushing, what do you perceive as the need for further treatment in this area? In other words, if these things are addressesed what would the likelyhood be of further recession in this patient (need for graft)?Thanks,
Dan MelkerSpectatorRon,
I answered your question in about 5 paragraphs and have no clue where it went. Briefly, the tooth is in labial version. This simply means that the root is in the position where the bone would be. Correcting the occlusion will not correct the lack of bone nor connective tissue in the area.
Benefits of connective tissue are:
1. avascular-prevents bacterial infiltration
2. dense connective tissue-prevents toothbrush causing recession.
Mucosal tissue has none of the above characteristics.
Choices of treatment:
1. Subepithelial graft-root coverage
2. Submarginal graft-increased connective on bone.
When there is recession and lack of connective bound down to act as a barrier, I always recommend soft tissue procedures.
I could spend hrs. showing you continued recession on teeth left untreated. Then I could show hrs. of treated teeth. Objectively, there is absolutely no comparison in long term health. Soft tissue treatment is so successful it is not funny. To date I have treated over 7,500 teeth and have probaly 7,490 successes. I am sure others have the same degree of success. I only tell you this because this is far and away the most successful long lasting procedure I do.
I would treat the above patient 100 out of 100 times.
Thanks,
Danny(Edited by Dan Melker at 4:14 pm on April 25, 2004)
(Edited by Dan Melker at 4:16 pm on April 25, 2004)
Dan MelkerSpectatorJeff,
I posted a comment accidently as a new topic. Frenectomy to graft or not to. Sorry.You can tell I am new.
If we can share I would like you to go to Dentaltown -Periodontal section-Topic-Altered Passive Eruption. This case is actually very similar to yours but rest. is involved.
There are all sorts of biologic cocerns I have when anterior crown lengthening with either a laser or scalpel.
1. Thickness of bone
2. Position of teeth-buccal or lingual position in bone.
3. Thickness of tissue-thin or thick
4. curvature of enamel at cej.
All these factors play a part in anterior cosmetic surgery.
If you are open minded let’s work together to achieve the best results for our patients.
Thanks,
Danny
BenchwmerSpectatorDan,
Both procedures were conservative, no restorations were involved. Both patients were new patients to the practice. On the Mand. frenectomy patient was told a graft may be needed in the future.
The Gingival reconturing case will be monitored over time, I always post follow-up photos over time.
The following photo is a 40 year old female, no perio problems, 3mm pseudo-pockets on facial #9 where gingiva is 3mm above CEJ. Bone sounds to 5mm,. I feel free to remove up to 2mm gingiva to reshape the gingiva on #9.
What concerns should I have?
Tx plan is a limited one tooth laser gingivectomy with the Nd:YAG to expose enamel. No restorations are planned.Jeff
AnonymousGuestQUOTEQuote: from Dan Melker on 4:13 pm on April 25, 2004
Correcting the occlusion will not correct the lack of bone nor connective tissue in the area.
Benefits of connective tissue are:
1. avascular-prevents bacterial infiltration
2. dense connective tissue-prevents toothbrush causing recession.
Mucosal tissue has none of the above characteristics.Danny, below I have outlined what looks to be attached gingiva in green. Tissue looks pink, stippled and firm. Other than ideal positioning of the tissue what am I missing here? Do you feel there isn’t enough attached gingiva? or that this just hasn’t been restored to ideal?

Thanks,
p.s. I saw your other post after this one and moved it.
Dan MelkerSpectatorJeff,
I cannot argue about bad perio or bad rest. dentistry. I do not think we are comparing apples to apples.
Let’s start with the frenectomy on mand. anterior. #24 has recession and the patient is young. the tooth is in labial version, this there is a very thin labial plate of bone if we are lucky. I would venture to say that there is miminal if any attahed tissue on #24. Probe the buccal sulcus, then probe the outer portion from coronal tissue to mucogingival junction. I will bet the #’s equal each other. Therefore there is not attached connective tissue bound down to either root surface or bone. After 29 yrs. of seeing these areas break down I would recommend a soft tissue procedure.
As far as the maxillary, let your 6 month followup be the judge. Let’s learn.
I believe in the laser even though I do not own one. Lasers will not cure all our problems. I will be happy to send you cases where proper periodontal procedures produced the ideal outcome with no root sensitivity, long teeth, black triangles, etc. occurred. These are advanced perio-rest cases.
Do not forget basic BIOLOGIC prin. when using your laser. I am not sure who your Periodontists are but frankly none of the above concerns of yours have never been a problem for me.
Let’s all learn. I would be very happy also to send you altered passive or active eruption cases for your evaluation. Similar to your case shown above. It may be a real eye opener for you. I love to learn and love to share, that is why I am here.
Danny
THIS case belongs with the FRENECTOMY TOPIC BY JEFF
Thanks
(Edited by Dan Melker at 5:30 pm on April 25, 2004)(Edited by Dan Melker at 5:35 pm on April 25, 2004)
Dan Melker
AnonymousGuestQUOTEQuote: from Dan Melker on 6:21 pm on April 25, 2004the tooth is in labial version, this there is a very thin labial plate of bone if we are lucky. I would venture to say that there is miminal if any attahed tissue on #24. Probe the buccal sulcus, then probe the outer portion from coronal tissue to mucogingival junction. I will bet the #’s equal each other. Therefore there is not attached connective tissue bound down to either root surface or bone.
1 more question if you don’t mind [well maybe more than 1 unless it becomes too obvious how extensive my perio training was 😉 ], What do you believe caused this to begin with? frenum pull? if not, what will keep the same thing from happening after the graft is in place? (With a graft the tooth position hasn’t changed and the amount of bone hasn’t changed.)
Dan MelkerSpectatorRon,
No question the problem was caused by labial position of the tooth as well as possible secondary occlusal trauma. Look at the wear of the incisal edge.
Look closely at your two green lines. If you look at the gingival one you can still see red tissue below the line. If you probe to the mucogingival junction you will get a #. If you then probe from green line to green line you will get a second #. They will be about the same. Therefore you have really minimal or no attached connective tissue.
The above benefits of connective tissue are the reasons to do soft tissue procedures. Over the last 17 years I have been doing subepithelial grafts. By and large they are where they were when I placed them. Some over 5-7mm. of reason covering the entire root. This is far from unusual. Actually quite the norm.
Connective tissue again by being avascular and dense is a great barrier and protects the underlying structures.
I found a slide from 1975. I will mail it with the other material. The followup is 1978. You can tell from the dates on the slides. Which way would you like tobe after 3 yrs. Also notice the change in papilla height between 24 and 25. You can be the judge. What some 29 yrs. ago. If people would learn from other peoples successes and failures it would make their lives so much easier.
This is really a simple case for an attached tissue procedure especially with the patients age. By the way I did multiple grafts on my son bfore ortho, so yes Jeff I would want one in my mouth if necessary. Also covered up an exposed root(#11) on my wife. She likes it, very cosmetic.
Danny(Edited by Dan Melker at 7:03 pm on April 25, 2004)
-
AuthorPosts
