Forum Replies Created
-
AuthorPosts
-
Kenneth LukSpectatorHi Glenn,
For the inflammed gingivae, I used 4w .02on/.03off. with irrigation; Slow movement.
For the healthy gingivae, I tried with 1 w cw no irrigation. Much quicker movement.
I’m still trying with different power and settings.
Ken
dkimmelSpectatorMy flight will not get in til after 7:55 PM. Looks like I’ll have to catch you guys later.
DAvid
vinceSpectatorNice pics Andrew.
The case with 2 ulcers side to side would have been a cool case to try the 2 wavelengths, one on each and then monitor, compare and contrast.
Regards
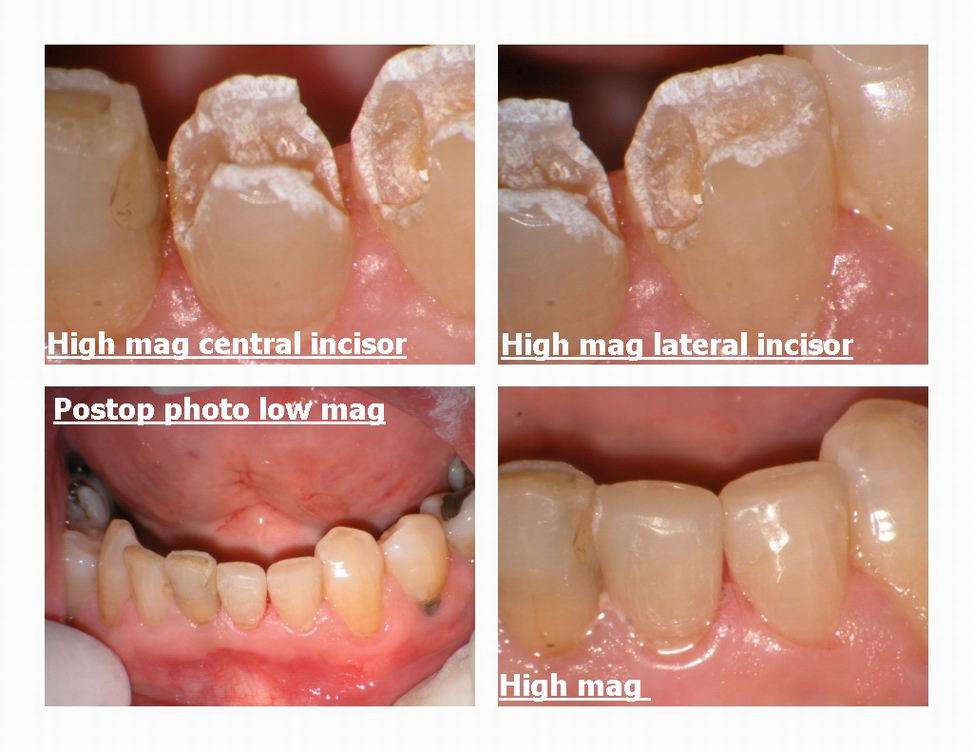
Glenn van AsSpectatorHi folks: Here is another simple case I did this week ( got lots of cases done this week dont know why) and it was a lower incisors case.
No anesthetic, patient rated pain as 0/100. Wedges were worst part he said.
Patient watched whole procedure on TV……was riveting he said.
Desensitized with Mark Colonna modified Delight technique…..high wattage defocussed for 2 mins
Full power for resins of which the mesial on the central was simple ( resin) and the others were most likely silicates or some old resin as they were a tough time.
Got them out and replaced with Palfique shade A3…..nice material.
Spherical particles and looks nice at end.
Just a simple thing like this makes huge impression on patient.
Took around 50 mins I think with photos.
Cya
Glenn

Glenn van AsSpectatorPs Patient now wants to do other side ( he only wanted the left side done before)……….
Thats the power of the laser and scope.
Glenn
BenchwmerSpectatorGlen,
I always wonder about the emphasis on hard tissues laser user on no anesthia. If I was doing this case with Hi Speed handpiece, I wouldn’t use any local and would still get no pain. Retreating anterior composites of this age, occlussal wear, there is no response.
Using the OpusDuoE, where I can vary Hertz, I have only had to stop and give local a handfull of times in cavity preparation/ caries removal.
Do you really need to pre-lase, expose the teeth to added energy, take the added time?
The results and preparation technique are wonderful, but why the extra laser exposure?
Jeff
Glenn van AsSpectatorJeff you always ask interesting questions!
If this is the patients first attempt with lasers then they will be much more apprehensive and in addition they will be difficult to calm down if they feel something.
THe extra laser time does NOTHING physically to the tooth at all, it only takes 2 mins of time and gives me a little more comfort. I have done Class Vs with this technique in the lower anterior at 30 Hz and 140 mj and the patient felt nothing during the preps. At the very end after polishing the resins etc, I noticed one spot that wasnt well done. The patient was relased at 30 Hz and 70 mj or half the energy I used before and the JUMPED ……..Ouch that hurts.
I hadnt relased for the two minutes and the energy was half of what I used before. She was very jumpy after that until I finished.
As for the Delight, it too has multiple and higher hertz settings than the Opus which I believe only has a maximum setting of 12 Hz and a higher maximum of 1000mj.
You need to use the higher energy settings because if you measure the energy coming out of the hollow wave guide it will only be something like 20 % of the energy that starts out from the box.
THe repetition rates available for the Delight erbium include 3, 10, 20, 25 and 30 Hz which give far more range and variability than any of the other lasers.
Correct me if I am wrong but the Opus is 3-12 hz isnt it?
The Biolase is 20 Hz.
To be honest , I rarely use anything less than 30 Hz on hard tissue except in deep preps as it slows down. For soft tissue and apthous ulcers I will vary the Hz rate more.
Finally, I am of the opinion that pre-existing resins and their age are of insignificance to the sensitivity of the patient. Existing depth of the restorations, patient age (pulp size) and patient individuality, as well as number of previous laser preparations seem to be bigger clues for me as to the potential sensitivity of the patient.
I do find that the age of the restorations may determine how easy they are to get out of the mouth with the laser. Higher filled resins and silicates are tougher to get out with the laser compared to microfills or sealants when using the same energy settings.
When I used the slowspeed to remove some Dycal (it wont come out with the laser, when I view it with the scope), the patient felt quite a bit.
In closing , alot of my thoughts come from seeing how the laser interacts with tissue at 10X power and above. Your experiences may of course be different and it is great to get alternative viewpoints.
Thanks for your post Jeff……..
Glenn
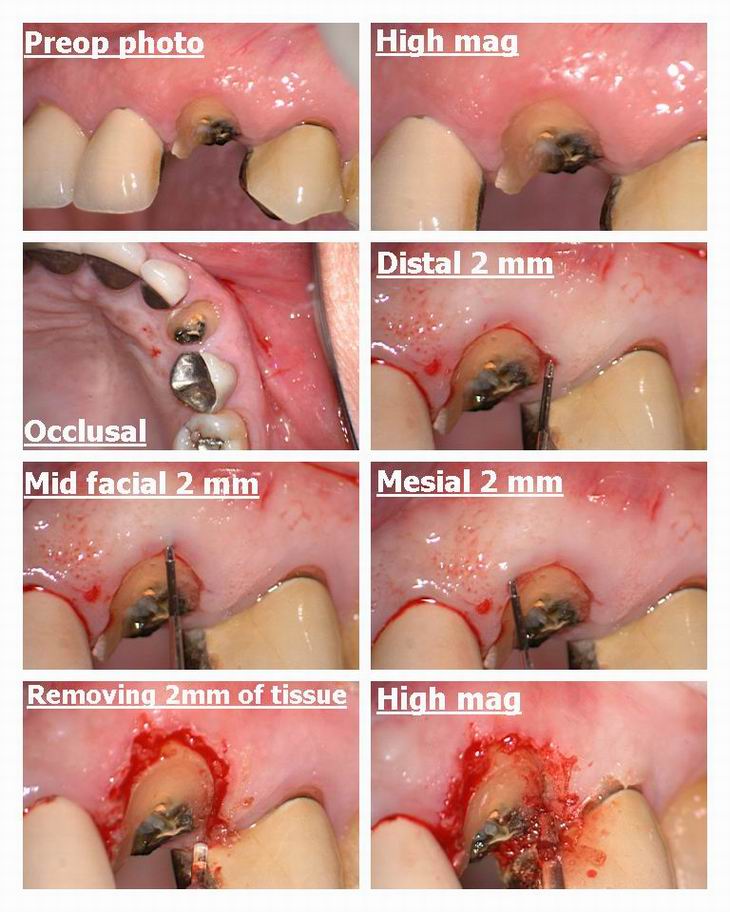
Glenn van AsSpectatorHi folks: Well I did this osseous case yesterday and made a few mistakes, one of which I didnt realize til the patient left and I looked at the photos.
FIrst off, this lady is 75 years old and fractured a canine crown off at the gingiva . THe lateral has a crown as does the premolar.
I had not met the lady but my associate had seen her and rightly decided that there wasnt enough tooth structure remaining to replace the crown but with osseous recontouring we would create enough.
Alternatives could have included an extraction of the root and 3 unit bridge or implant. Positives of trying to retain the tooth included better flossing than a bridge and less cost and time than an implant. Others may have chosen one of the other treatment plans.
I had another colleague in watching the procedure so I was a little distracted when doing this but all the same here are the results.
First off I know that the canine will be longer than the other teeth at the gingiva and in addition that there will be recession on the adjacent crowns.
I used a 80 degree tip to remove some tissue first so the flap wouldnt go back to where it was before. I used 30 Hz and 100 mj for the soft tissue.
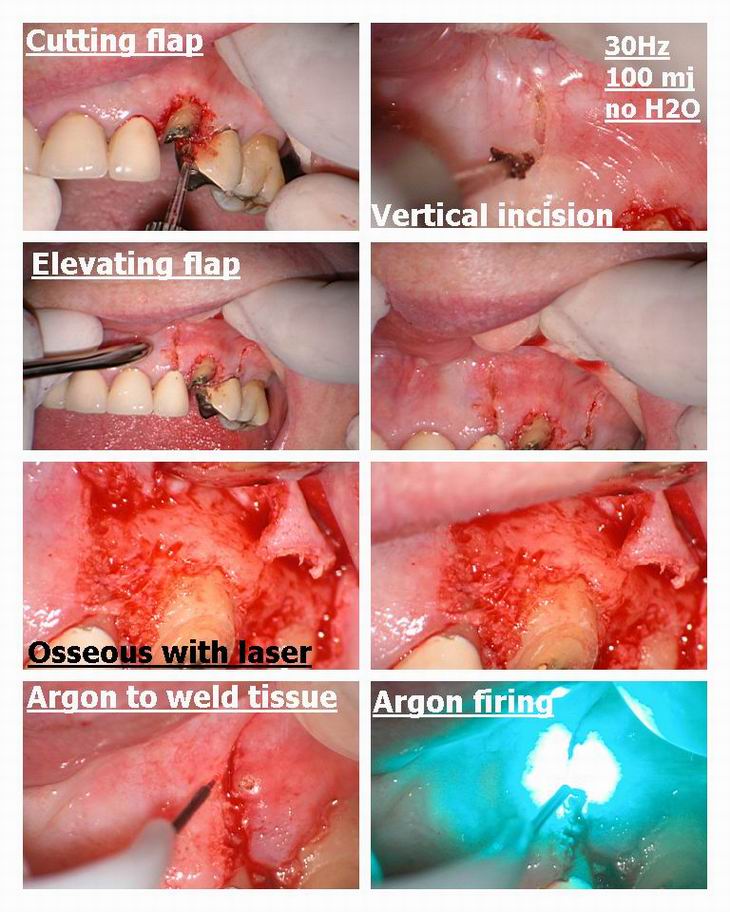
Then we elevated the flap. I had broken my chisel tip (large tears flowing now) the day before so I had to use the soft tissue tip (pointed ) to cut the flap and releasing incisions. The flap was raised and at this point I forgot to take a bunch of photos, but the final photo shows the bone removed and the flap replaced. For bone I used 30 Hz and 160 mj with water and a 80 degree 600 micron tip.
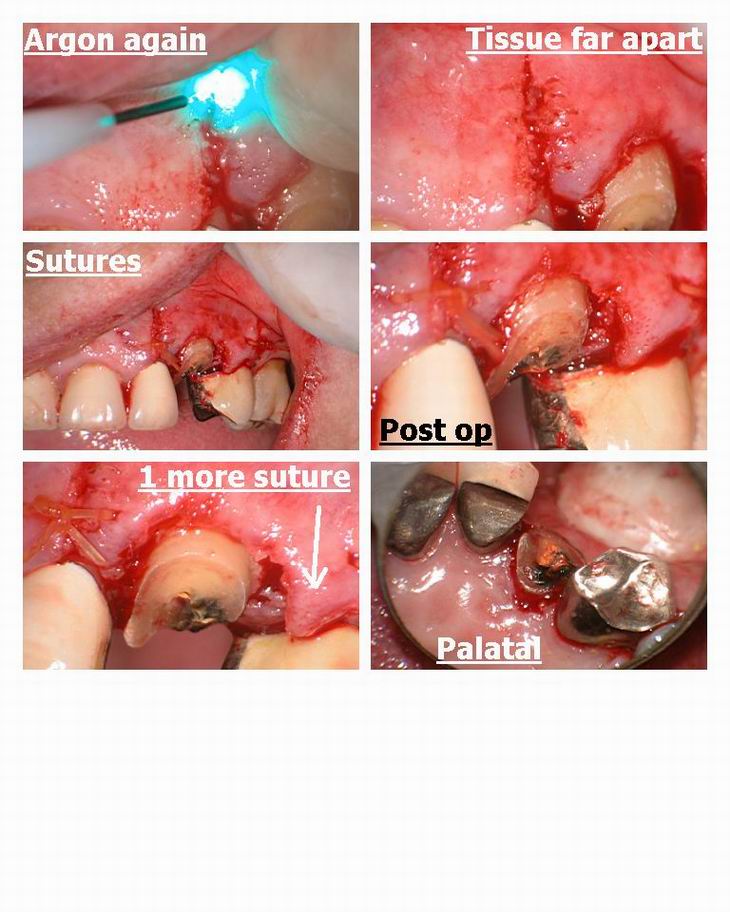
I tried to use the Argon to tissue weld but the tissue was too wide apart and it couldnt be reapproximated. I wonder whether its the tip that cuts a cleaner flap or settings I used.
Anyways I should have placed one more suture in the tissue but didnt see it til afterwards so I hope it will heal.
LIke I said , some you win, some you dont , and I think I could have done a better job with this one but time will tell.
Fire away with suggestions as I am trying to improve my technique. I want to get some smaller instruments and smaller suture as well……….it looks horrible under the scope, reminds me of tug of war rope.
Cya
Glenn
dkimmelSpectatorGlenn,
Couple of questions and thoughts.
What is her lip line like?
Some of what I see maybe because of the photos. One concern I have is if you have enough reduction. You will end up with about 2mm of tooth to work with when this is healed. For a canine this is pushing it. I understand esthetics would be compromised more by being more aggressive. The interprox reduction looks even less.
Another concern is the placement of your releasing incision. Generally I prefer to go to the line angles to release as you get more recession if you relieve over a root prominence.
On restoring I would make sure she was in group function on that side and was given an NTI or the splint of your choice. Unless trama was the cuse of the fracture, I would be very concerned about a parafunctional activityOn your posting of photos, did you upload each individualy or as a colllage? What is your file size for the images?
Great posting!
David(Edited by dkimmel at 4:07 pm on July 19, 2003)
AnonymousSpectatorGlenn,
Like David, I also usually do my incision a little differently. I’d split the papilla between 9/10 and also 10/11 and angle outward as I went more cervically(apically?) so the base of the flap is wider than the top.This keeps the flap with a very good vascular supply. You also then have the choice of suturing across the labial as you did or going interproximally. I think this way, recession on the adjacent teeth shouldn’t be much of a concern.

You definitely had some tough choices regarding esthetics and ginigval levels. I’m guessing since the tooth fractured and there appears that there used to be a pretty large restoration, that the canal was pretty calcified,pt age, and endo /post/core (with the crown lengthening) wasn’t a good option?
Wouldn’t we all have a chance at being master dentists if we could see and discuss the things we see in everyone’s post pictures, before we actually did the procedures?

Thanks for posting, Glenn- I know that after 20 years I find its easy to find myself running on auto-pilot in the office and due to your generosity in sharing, I know that there will be so much more for me to consciously think about before tackling the next fractured tooth that walks in my office.
vinceSpectatorHi Glen,
Great case as per usual.
I concur with David and Ron regarding the position of the vertical incisions and the amount of osseous reduction, especially at the line angles. I assume that the palate had enough BW.
Awesome pictures and very innovative regarding tissue welding, do you know how to with the 980 diode? I assume its tough to remain in that temp window to allow this. I have never seen/used a ‘chisel’ tip. How does that work?Best regards,
ASISpectatorHi Glenn,
My concerns echo those of the others:
1. Position of vertical incisions ought to be closer interproximally to avoid gingival recession tendency upon healing. Sometimes if one interproximal aspect requires less osseous relief, I will even just do one vertical incision to minimize recession and to keep the site as noninvasive as possible. It would be ideal if the mesial aspect is not disturbed if I had the choice.
2. Insufficient osseous relief of the canine
What is the suture size used? Material?
I applaud you for showing and sharing your case. Not many will with the gall and the balls to exhibit their less than perfect treatment for all to see. I tip my hat to you. This is one of the many qualities that I admire about you.
Andrew
SwpmnSpectatorQUOTECorrect me if I am wrong but the Opus is 3-12 hz isnt it?I believe the Hz range on the OpusDuoE is 7 to 20 pps.
Very nice composites.
Al
ASISpectatorHi Fellow Forum Folks,
A couple of Cl 5 composite treatment on #44 and #45.
Preop is photo 1.
Photo 2: Prep by DELight 600u 80 degree tip with dentin and caries setting. #44 gingival troughing by DELight 600u 80 degree tip at 25Hz 35mj dry with air coolant along long axis of tooth. #45 gingival troughing by Biolitec 980nm 600u at 1W CW dry with air coolant
Photo 3 is post-op. Restored with 3M ESPE Supreme.



Andrew
SwpmnSpectatorThat’s a cool case. I think the Erbium is better for apthous ulcers due to shallow depth of penetration. More comfortable for patient especially when you can turn the Hz way down as with your DELight.
What camera? Flash system or dental operatory light?
Al
-
AuthorPosts
