Forums › Diode Lasers › General Diode Forum › Laser Perio
- This topic is empty.
-
AuthorPosts
-
whitertthSpectatorBob Et al,
I would like some clarification on how results are obtained by using a diode to decontaminate pockets..
What I mean, is that What is actually happening in the pocket to cause pocket shrinkage( Since I see that using my diode)….How does that differ from the Nd Yag.? When u would if at all expect to see relapse with a diode? How does it differ with the Yag? Would either hold up in a court of law as acceptable treatment for a moderate perio trditional surgey case? Can these results be achieved with the ER wavelenghth? I have not been able to reproduce anything like what I see with my diode with my Warerlase…..
Ok gang This a new one to keep us busy for a bit….If u use the diode go over your procedure…(Edited by whitertth at 1:08 pm on May 26, 2004)
Robert Gregg DDSSpectatorHey Ron,
I’m gonna let some diode/PerioLase/erbium owners describe the difference between the clinical results they have seen.
But here’s my general take on it.
For example, Diodes:
1. Are “hot” lasers and tend to create a dry versus a moist wound at higher settings.
2. Kill some bugs. Mostly on the tissue surface and not a depth of 2-4mm. Not all or most, but enough to allow the body to recover and heal.
3. At lower settings, there is less dryness and more moisture in the tissue, germ lethality is much less.
So there is a trade off with a CW/gated diode in controlling the desired effects.
Alternatively, the Free Running Pulsed Nd:YAG (Periolase):
1. Has intensity in each pulse of 100 millionths of a second (and 2000 watts per pulse) for substantial germ lethality at depths of 2-4mm and through “priviledged sites” that anaerobes hide in (Harris, Loomer AADR 2003). PS are endothelial cells, macrophages, calculus, dential tubules (Koch).
2. That intensity (brightness) is offset by pulse “off” times that are about 500 times longer than the on time. At 20 hz that would be 100 usec on and 49,900 usec off. That allows the tissue to cool down a bit and not burn or get too hot.
3. Long pulse durations are user selectable (150 to 650 usec). Because the tissue and most importantly, the blood is not boiled (vaporized) away at long PDs we can “slow cook-it” or poach it (blood) if you will. This allows the blood to form of heat thrombus that sticks to the connective tissue and root surface, which seals the pocket from the oral environment and epithelial migration. Thrombi have nutrient cells in that zone of thermal injury called the “stasis” zone (as in “hemostasis”–NOT coagulation, which is cell death). Thrombi later converts to fibrin, the elixer of regeneration!
For comparison, erbiums:
1. have no selectivity within tissue.
2. so bone, PDL, cementum all get to absorb the wavelength along with any bacteria. But again, the bacterial kill will be on the tissue surface, not at any depth into tissue as Harris describes:
http://iadr.confex.com/iadr/2003SanAnton/techprogram/abstract_27983.htm
3. No hemostasis means no thrombus, no fibrin, no regeneration.
So the healing that we do see when we get some results with diodes or even erbbiums is “repair” not regeneration.
Repair = Long junctional epithelium. Long JE is still health and is clinically acceptable, but it may not be as stable as true regeneration. It is certainly not our end goal we want.
We strive at all time to achieve:
Regeneration = New Attachment. NA = new cementum on the root, new PDL, new alveolar bone.
http://iadr.confex.com/iadr/2004Hawaii/techprogram/abstract_47642.htm
The first and only human histology (the highest form of evidence) showed 6 of 6 teeth treated with LANAP and FRP Nd:YAG had 100% cementum-mediated new attachment with new bone at 3 months post op. These were the first 6 teeth ever subjected to this protocol and then removed en bloc and sectioned for microscopic evaluation.
Okay Ron Schalter, your turn!
Bob
whitertthSpectatorBob
This is why I love u….great answer to a good question…this thread should make some good reading for a while….I really like this board and am proud to be a member, contributor, and participant….The information on this board has really expanded my laser knowledge and I hope I have helped others. For the newer members, post your thoughts, ask alot and dont berate others…….Many of us laser pioneers have attempted forms of treatment that was deemed crazy and now they have paved the way for others using lasers today….Okay ..enough of the nostalgia…lets keep this interesting thread going…..
ASISpectatorHi Bob,
Great encapsulation of the 3 different wavelengths on periodontal treatment.
You are forever the teacher. Your words and explanations are poetic in nature. Concise and precise.
Andrew
Robert Gregg DDSSpectatorQUOTEQuote: from ASI on 2:51 am on May 27, 2004
Hi Bob,Great encapsulation of the 3 different wavelengths on periodontal treatment.
You are forever the teacher. Your words and explanations are poetic in nature. Concise and precise.
Andrew
The result of YEARS rambling on and on and on……..to whomever would listen!

Thanks for the nice comments Ron and Andrew.
Bob
AnonymousGuestQUOTEQuote: from whitertth on 1:06 pm on May 26, 2004
Bob Et al,When u would if at all expect to see relapse with a diode?
Hi Ron,
In the time I used my diode (~9 months) to treat perio the cases that relapsed did so because of 3 factors which added together overcame what the patients body could handle.
1. less than great OH
2. systemic factors (diabetes was significant in 2 relapses)
3. occlusion/ bruxing
I believe like Bob, that the diode tx is really just getting Long JE and will not hold up as well to the insults our patients throw at it , as the new attachment/new bone will.Here’s a case I just saw recently (this will look familiar DAvid K) about 9 months after FRVP nd:YAG tx.
The frvp nd:yag
69 YOWF Severe crossbite. Bilateral distal extention RPD.
Furcation involvement 10 + mm distal pocket mobility
9 months post Tx – 6mm distal pocket/ no mobility . Appears to be bone fill in furcation and some distal. Pt OH not as good as it should be. Will reevaluate for return nd:YAG Tx at 3 month recall.
Maybe Mark C. can get Bob Barr to post some cases. I just haven’t seen any with bone fill.
whitertthSpectatorIs there any chance this is Perio endo type lesion? Have u pulp tested or anything like that ?Maybe that lesion fills somewhat with a RCT?
AnonymousGuestChecked the chart -negative to percussion, normal limits hot, slight sensitivity cold that didn’t linger.
Robert Gregg DDSSpectatorRon S,
Thanks for the post. Clearly some bone fill–especially density.
I’d suspect some hard to find occlusal interences if that doesn’t completely fill in and get more dense.
RCT is still a possibility in some of these. But surprisingly few of these are endo related.
Just saw one today 1.5 years post op that I Tx planned for RCT. Today tests 33 on EPT and the bone fill, WOW!
I’ll post later.
Bob
Robert Gregg DDSSpectatorOK here we go.
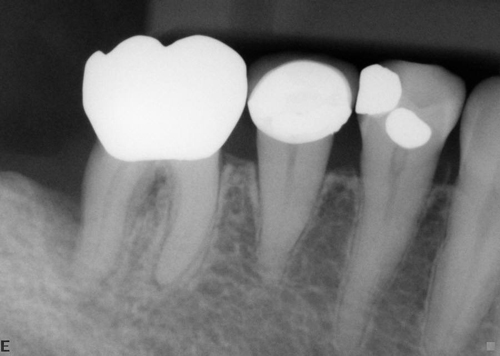
First image is pre op:
10-03 Pre Op x-ray. There is no evidence of much bone on the distal and the apical area looks to be involved.
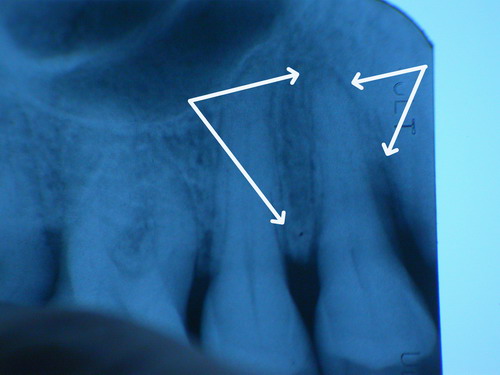
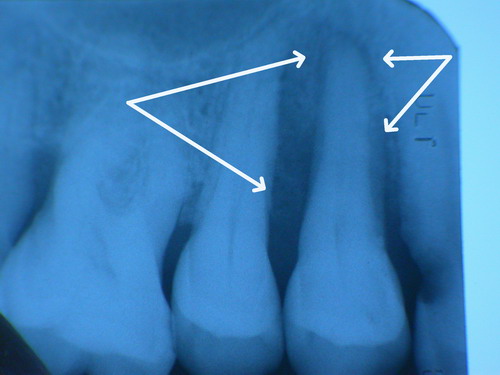
5-04 (9months) Post Op. Distal area is clearly corticated and very dense. Apical area is much improved. Mesial area did not respond as well. There is a soft tissue defect suggesting granulation tissue was pulled out. Also, occlusion was still hitting hard today and was adjusted on the buccal incline planes and the MESIAL marginal ridge!!
Again, the tooth tests “vital” at 33 on the EPT, and “ache” with FRP Nd:YAG at 4.00 watts 150 usec, 20 Hz in contact with facial enamel for 15 seconds that immediately went away with its removal…..
Bob
Lee AllenSpectatorBob,
I am pleased to see that you have included the FRP (Free Running Pulsed) prefex to the NdYAG since your contribution to my understanding is that it is the key to the perio effectiveness of the Nd YAG.
How much for a used one?
AnonymousGuestQUOTEQuote: from Robert Gregg DDS on 4:32 pm on May 27, 2004I’d suspect some hard to find occlusal interences if that doesn’t completely fill in and get more dense.
Bob
Bob,
A little more info- patient at time of FRVP nd:YAG tx had just been placed in a U/CD and L/RPD by prosthodontist. I’m inclined to think it may be torquing by the distal extention RPD (which has a metal base), although I couldn’t seem to get much movement out of it. In your experience does that sound reasonable as opposed to traumatic occlusion from u/CD? I did get bleeding on probing on the distal so we’re going the try to improve OH for the next 3 months, then reevaluate.
Robert Gregg DDSSpectatorQUOTEQuote: from Lee Allen on 9:12 pm on May 27, 2004
Bob,I am pleased to see that you have included the FRP (Free Running Pulsed) prefex to the NdYAG since your contribution to my understanding is that it is the key to the perio effectiveness of the Nd YAG.
How much for a used one?
Hi Lee,
Good to hear from you.
The only “used” Periolase lasers are………in use by dentists.:cool:
Besides, it’s the investment in knowledge and understanding through training that lists at ฿,995. The PerioLase MVP-7 is FREE with training! 😉
Our problem is we don’t have enough Periolase lasers to use for our upcoming clinical research study, so we will have to build new ones for that.
The one used Periolase we have is the result of a shipper putting the tong of a forklift through the box, the bezel cover and into the PerioLase. The laser still worked!!. No optics or alignment problems.
The dentist was using it until we could get a new one built. Shipper’s insurance paid for the bezel cover replacement and repair of suspect (but functioning) electronics.
That’s what it takes for us to get a used one!

Take care,
Bob
Robert Gregg DDSSpectatorQUOTEQuote: from Ron Schalter DDS on 10:13 pm on May 27, 2004
Bob,
A little more info- patient at time of FRVP nd:YAG tx had just been placed in a U/CD and L/RPD by prosthodontist. I’m inclined to think it may be torquing by the distal extention RPD (which has a metal base), although I couldn’t seem to get much movement out of it. In your experience does that sound reasonable as opposed to traumatic occlusion from u/CD? I did get bleeding on probing on the distal so we’re going the try to improve OH for the next 3 months, then reevaluate.Ron,
Yes, that makes more sense. In my experience PDs can torque teeth unfavorable to regeneration.
Look, for example, at the PDL space on the bicuspid. The mesial is thicker towards the apex, and the distal is thicker towards the crown. There is an occlusal trauma hitting the tooth to cause that tooth to fulcrum in that way.
I suspct there is a heavy distal marginal contact.
Similar with the molar. In my experience, there is a heavy mesial marginal contact on the molar driving the tooth (orthodontically) down into the alveolus, together with a distal marginal ridge trauma on the proximal bicuspid. See if you can find it. Look very closely for them. You may need green articulating wax.
Bob
Dan MelkerSpectatorBob,
Exremely impressive! It would be great as we talked before if you could do a small flap and take a picture! I doubt you would see anything other then alot of new bone! Just awesome.
I am alittle uncomfortable with Ron’s case because of the angle of the x-rays. X-rays can be misleading and that is why a minor flap and picture can be invaluable.
Either way there is no denying something very good is happening. That fibrin clot must be doing its job! Truly something to be very very proud of!
Bob, your posts are really impressive and really adds alot of credibility to the laser world!!!!
Thanks,
Danny
Ron and Bob-good things happen to people that try to better our profession!!!!!!! -
AuthorPosts
