Forums › Diode Lasers › General Diode Forum › Laser Perio
- This topic is empty.
-
AuthorPosts
-
kellyjblodgettdmdSpectatorI’d like to clarify something that Lee mentioned. As I understand it, it’s not just that the Periolase is FRP that is significant (although it is relatively significant) but that the pulses themselves are variable in their pulse-width.
I just got my Periolase two weeks ago. I have been trying for two years with my Pulsemaster (fixed pulse-width of 150 usec) to gain adequate and CONSISTENT hemostasis. It can’t be done. This week I treated an acute perio abcess using the periolase. The 650 usec pulse width makes it so much easier to predictibly “seal” the pocket to allow for healing.
Also, I would love to add that the ~โK you pay for the laser is totally worth it just for the training. I know Bob sounds great on here, but in person……Man, I was impressed!
Thanks, Bob, for not only educating us constantly on this forum, but for providing a technology that so significantly benefits our patients.
A note to Danny – Seeing the bone with a mini-flap would be great, but a huge part of the LPT philosophy is to avoid the “cutting” that the patient’s want to avoid. Perhaps in the future we will have better diagnostic imaging capabilities availabe to determine changes in bone quality. (Optical Coherence Tomography, maybe?)
Great Thread – Thanks for kicking it off, Ron.
Kelly
Dan MelkerSpectatorKelly,
I agree with what you are saying though in the beginning of any new trt. the more proof you have the easier it is to convince people of what you are doing and the success you are having.
An example, when I first started using Emdogain I told every patient I was going to open the area up free of charge to see what was present-did they get their money’s worth. I have opened up approximately 150 sites. Bob Gregg has seen the results. What I am saying is no one can disagree when they can see for themselves. Early on we should do things to learn and share our material.
Thanks,
Danny
Robert Gregg DDSSpectatorGreat discussion, everyone.
I appreciate the kind observations and comments from both Danny and Kelly.
I have taken Danny’s desire to get a picture of what is going on with a flap to heart. To be sure, the goal of LANAP is a closed procedure. But we are also trying to show the world what we are getting at this early juncture.
I told Danny that I would keep an eye-out for cases where I might raise a flap and take a picture. With a microscope and magnification, I bet I can do that with a very small incision. With the bone as high as it is on this tooth, that ought to be accomplished without any detriment. I also need to anesthetise this tooth and examine why the mesial has not done better. I can take a photo of that while looking under the scope.
I’ll see what I can show………more later.
Bob
Dan MelkerSpectatorCommon problem with mesial of maxillary first bi’s. Either bifurcations or furrows. Bob, tough place to get bone regeneration. Could calculus still be present in the furrow? I do not think the laser could have done better with the root configuration.(x-ray of #5 mesial)
Just unbelievable what you are doing!
Danny
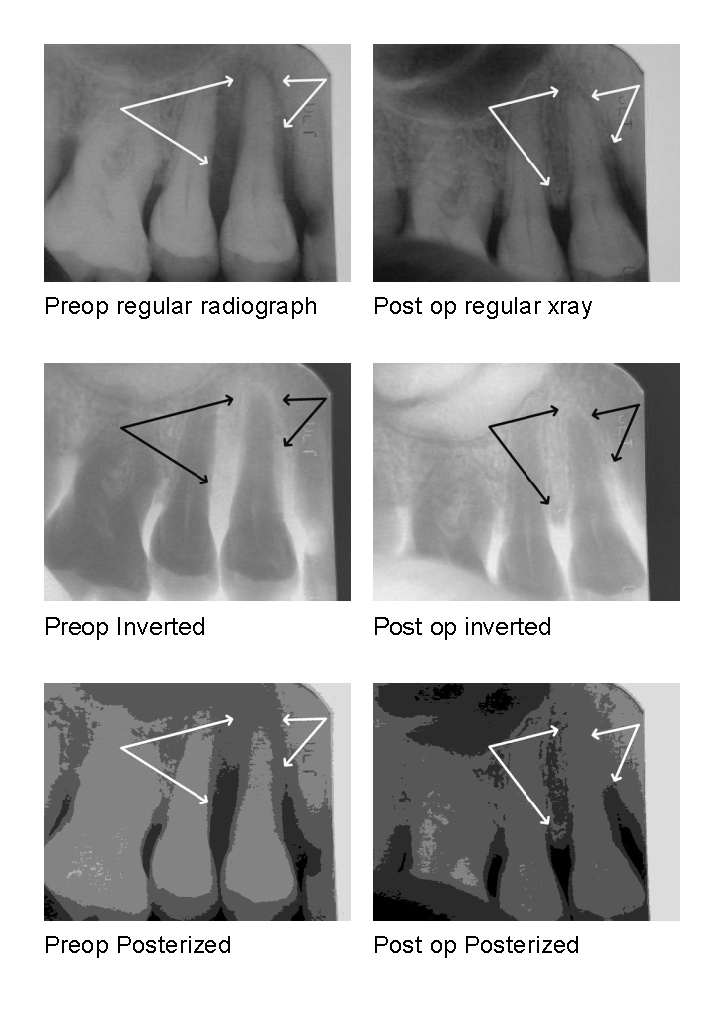
Glenn van AsSpectatorBob I color corrected your images and also played with them a little in my editor to invert them – neat huh and also posterized them.
The color scale for xrays should be desaturated or in black and white to get the right colors. Scanning them does what you did (or taking digital photos of them.)
This reminds me that if you have xrays you want to digitize , just take you camera , put it into macro mode (and Black and white mode if you want) and take the picture with the xray on a view box in a dark room and you can really nice quality , and you can zoom in on one part of the radiograph a little as well.
Here is the manipulation of your wonderful case and in closing I want to mention that this has been one of the most productive weeks here with people like Jeff, Ron, Sam , Bob and my very good friend Andrew all posting cases with pics and oh ya Kimmel as well but his pics would have been ALOT better if he had taken them through a scope- but I digress.
I have learned a ton this week in a great setting and I wanted to thank you all for showing us your cases, warts and all. The best way to learn is to see these cases in a visual format. Kudos to you all for a wonderful week.
Glenn
Robert Gregg DDSSpectatorDanny,
Yes, I think you are right about the mesial. I appreciate your thoughts and insights.
I do have a piezo tip for getting into the concavities (looks like ? with a ball on the tip), but even still some calculus doesn’t break free or even clean defects regenerate–especially if the laser disinfected granulation tissue matrix is removed.
I am still interested in the residual occlusal trauma that I observed at 9 months post op. That was adjusted and I need to see if I need to do more.
Is there a fracture to observe? I need to see……..
Having said that, I will tell the patient that I need to numb it up and make a small incision to take a peak at what might be going on in the furcation. I will take pictures of the mesial and the distal to show exactly what is there, warts and all as Glenn would say.
Glenn!! Dude!! (as Kelly would say;) )
What a great display of photo-“wurks”! Excellent presentations!
Clap, Clap, Clap!!!
You are exactly right–I took those two images quickly through the microscope and the Nikon CoolPix using the x-ray box for illumination. I didn’t color correct through any software.
So, thanks for the presentation and the tips on how to take better images. Greatly appreciated!!
Good stuff everyone–and not just back-slapping.
Bob
AnonymousGuestBob, I think I’m following what you say about the forces except on the mesial/apical of the bi.(question mark on image) Wouldn’t I expect something similar to the distal cervical on the bi, at the mesial apical 1/5? Or is, the widening you refer to, in the 2nd 1/5 from the apex? If so, does it show here instead of at the apex because of the curvature?

Thanks for your help on this,
Robert Gregg DDSSpectatorRon,
Keep in mind we are looking at a 2 dimensional view of a 3D object. There just may be a PDL space thickening more to where you would expect if you could look at a bunch of angulations.
The point is that there is PDL thickening at the distal-crestal (as you have higlighted), and just up from the apex on the mesial is some corresponding thickening. Go up even higher on the root towards the mesial crestal and the PDL thickening there suggests there is the rebound or rock-back from the tooth jiggling back and forth.
It isn’t so much that it is definitive evidence, but contributory info that helps to diagnose. It gives you a clue to what and where to look for a problem. Once you try to depress the tooth in the direction of the PDL thickening, put some art. paper to it, and maybe some green art.wax, you may see the exact 3D pattern of pressure on the tooth.
After all, isn’t a pocket just a really thick PDL space???
Bob
SwpmnSpectatorQUOTEHere’s a case I just saw recently about 9 months after FRVP nd:YAG tx.
9 months post Tx – 6mm distal pocket/ no mobility . Appears to be bone fill in furcation and some distal. Pt OH not as good as it should be. Will reevaluate for return nd:YAG Tx at 3 month recall.I must say I’m amazed at this case. No disrespect to Gregg and McCarthy but a presentation by a user not associated with the company is most impressive. The improved angulation of the post-op radiograph appears to strengthen the clinical findings.
Why would a “return Nd:YAG treatment” be indicated? I thought I had understood that it was not necessary to retreat sites with the Periolase?
Al
AnonymousGuestAl,
2 reasons for possible retreat-
1. poor oral hygiene
2.in my limited experience (little over 1 year), sometimes double digit pockets need 2 treatments [its a secret so don’t tell anybody ;)]
Robert Gregg DDSSpectatorHi Al,
Good to hear from you. Great question.
The reasons for retreat are simple and the same as any other retreatment of say and RCT–not all of the etiology was addressed at the first time of treatment:
1. Occlusion
2. Calculus
3. Furrows
4. Enamel pearls
5. Untreated endo/perio combo lesion
6. Root concavities
7. Root fractures.
8. Removal of granulation tissue (needed to provide scaffolding)To name of few.
There is no need for repeated retreatments one week or one month apart to “tease” the tissue up coronally by repeated de-epithelializations and decontamination appointments. Very inefficient chair and operator time as well as unpredictable clinical results.
One treatment, one appointment, one fee (crown fee +20% is fair) then evaluate 6 to 9 months, just like an RCT. Did the bone come back? No need to retreat. Did an area not respond as expected? Time to address what didn’t happen. Experience leads to more predictability and reproducible and expected results, like in the distal of #5. Inexperience leads to incomplete results–like the mesial of #5. That’s OK. That’s why it is the practice of dentistry, not the perfection.
When Del and I started out, we didn’t get the results we get today either.
By the way, the bicuspid case I posted WAS done by someone not associated with the company. Neither Del, nor I treated this patient. It was treated by my now departing associate. I just did the post op on a patient I had never seen previously for any reason. We neither coached the associate nor consulted him on this case. The first I ever saw it was the day I posted the x-rays for a 9 month follow-up.
All the best,
Bob
SwpmnSpectatorRon and Bob:
Thanks for the clarification. Indeed it appears that the bone “Did come back” in Dr. Schalter’s case so perhaps no need for retreatment?
Question on retreatment – should there be a fee or is the initial fee adjusted to cover any necessary secondary LPT?
Bob:
Questions on retreatment reason number 2 – calculus:
Although I have seen a computer animation of LPT, when Mr. Schaeffer made his presentation the notebook battery died and we were not able to completely view an actual surgical video. No fault of Mr. Schaeffer’s but “Hooters” is not known for its scientific presentation facilities.
If we are not reflecting a complete flap does it not make it difficult to visualize and remove all calculus? I think I remember the periodontists told me years ago one of the reasons they reflect flaps was to remove all calculus. However, think I’ve also read that even with reflected flaps 100% of calculus is still not removed.
If we are not able to remove all calculus with LPT(or at least less than that removed with conventional flap reflection), is there evidence that the calculus is somehow altered or “sterilized” so that PDL and osseous regeneration is facilitated?
Mr. Schaeffer indicated that the first pass with the Periolase Nd:YAG alters calculus so that removal with the piezo-electric scaler is facilitated. Can you offer an explanation as to how the Nd:YAG makes calculus easier to remove?
As a further question, what are the advantages of using a piezo-electric scaler in LPT when compared to an ultrasonic scaler?
Maybe too many questions but I must admit this is the most interesting thread I’ve seen on LDF in quite some time!!!
Al
SwpmnSpectatorQUOTE8. Removal of granulation tissue (needed to provide scaffolding)Bob:
One more question as I once again expose the fact that I’m not the “sharpest tack in the box”:
What is “scaffolding”?
Al
dkimmelSpectatorThis has been a great thread!!
Allen :As a further question, what are the advantages of using a piezo-electric scaler in LPT when compared to an ultrasonic scaler?
I can tell you that when we use the perioscope you can rapiedly see the difference between the Piezo vs the ultrasonic scalers. The tips are far smaller and diamond tiped. The motion is different. Hands down the Piezo is more effective in calculus removal. It is also more comfortable to the patient. ( Note All Piezos are not created equal.)David
Robert Gregg DDSSpectatorRon?
Where did the “reply” button go???
QUOTEQuote: from Swpmn on 7:42 pm on June 2, 2004
Ron and Bob:
Al
Al–You are asking excellent questions! See my remarks below your questions pasted below:
Ron and Bob:
Thanks for the clarification. Indeed it appears that the bone “Did come back” in Dr. Schalter’s case so perhaps no need for retreatment?
That’s where the professional judgement comes in while looking for clinical signs and symptoms of rebound disease, which are VERY subtle inthe early stages.
Question on retreatment – should there be a fee or is the initial fee adjusted to cover any necessary secondary LPT?
1) It can depends on the depth of the original defect. “Double digits probed depth “require” double treatments”–but not until 9-12 months have passed to assess the initial healing. At least, that is what the patient is told during the initial consult.
2) Is the patient’s response to treatment symetrical in that all areas responded similarly (good or bad)?
That implys a host-dominated response to LPT treatment (i.e host immue response, home care, compliance, genetic predisposition, etc).
Was the healing asymetrical in that some areas healed extremely well and other areas on the tooth or in the mouth not heal as well?
That suggests that there may be a practicioner/operator deficiency in technique (i.e. residual plaque, removal of too much granulation tissue, failure to get intial closure with the long PD, etc)
It also might suggest a patient co-factor (i.e. root fracture, enamel pearl, poor root anatomy, etc)
So, generally, symetrical healing is what we are striving for. Symetrical breakdown typically is the patient’s responsibility and retreatment is full fee. I have a few patients, 8 to 10, that just don’t respond to any treatment in the sense of long-term health, and need LPT every 2 years or so. Lifestyle and genetics are the dominant controlling factor in these patients based on my experience. At least we are working with the same tissue height as previous treatments since no tissue was removed.
Asymetrical healing is typically the result of something not attended to by the operator–almost always it is failure to adjust occlussion aggresively enough. Next contributing factor is residual calculus, then root anomolies/fractures. Depending on the reason for asymetrical healing, we charge for retreatment per tooth–about ๯ per tooth. If I find occlusal trauma or calculus, I don’t charge he patient, and surprise the patient at the end of the appointment by not charging them.
Tooth #5 in my associate’s case is an excellent example. The distal healed perfectly. The mesial did not. Asymetrical healing!! Why? It’s the clinician’s job is to find out. Healing and health is the expected result in LPT, or RCT, or broken bones, or ruptured ligaments or whatever. Delayed or partial healing in the human body is not the natural state of affairs, so why?
Bob:
Questions on retreatment reason number 2 – calculus:
Although I have seen a computer animation of LPT, when Mr. Schaeffer made his presentation the notebook battery died and we were not able to completely view an actual surgical video. No fault of Mr. Schaeffer’s but “Hooters” is not known for its scientific presentation facilities.
The computer amimation is a generally descriptive, not instructionally accurate.
If we are not reflecting a complete flap does it not make it difficult to visualize and remove all calculus? I think I remember the periodontists told me years ago one of the reasons they reflect flaps was to remove all calculus. However, think I’ve also read that even with reflected flaps 100% of calculus is still not removed.
Correct. LPT is a “blind” procedure, and does challenge the operator to use other senses than the eyes–like tactile feedback. But make no mistake about it, raising flaps does not insure the removal of “all calculus”. The perio literature is clear on this. The Annuals of Perio–the AAP bible on perio truth–tells us as much as 50% residual calculus is left behind in even the most rigourous and controlled experiemental conditions–yet very positive response to conventional perio treatments is obtained! Why? Because we are reducing the critical mass, the bio-burden, to a threshhold that the host can now deal with and marshall its defenses to attack and heal.
If we are not able to remove all calculus with LPT(or at least less than that removed with conventional flap reflection), is there evidence that the calculus is somehow altered or “sterilized” so that PDL and osseous regeneration is facilitated?
Yes. The UMKC studies conducted largely by Charles Cobb’s research team over 10 years ago showed the FRP Nd:YAG passing by and over plaque and calculus altered and rendered the calculus sterile, while vaporizing the plaque.
Mr. Schaeffer indicated that the first pass with the Periolase Nd:YAG alters calculus so that removal with the piezo-electric scaler is facilitated. Can you offer an explanation as to how the Nd:YAG makes calculus easier to remove?
Yes. Lin (or Liue?) in Australia showed the FRP Nd:YAG altered/denatured the glycoproteins that attach plaque and calculus to root surface enough through scattered 1064nm irradiation to cause a reduction in “working strokes” by 50%.
As a further question, what are the advantages of using a piezo-electric scaler in LPT when compared to an ultrasonic scaler?
Piezos work linearly (back and forth) whereas magnetorestrictives work in a figure 8. Figure 8 tends to “lift-and-bang” against the tooth, and creates areas that skip over calculus. Piezos tend to “carve”. Amplitude is more constant and there is excellent tactile feedback with the smaller tips that magnetorestrictives just cannot duplicate. Piezos have smaller, longer tips for better access (think endo tips) and have more energy as well.
Maybe too many questions but I must admit this is the most interesting thread I’ve seen on LDF in quite some time!!!
Al
No problem. Anytime Al.
-
AuthorPosts
