Forums › Nd:YAG lasers › General Nd:YAG Forum › Surgical2
- This topic is empty.
-
AuthorPosts
-
etienneSpectatorHi Guys, apologies to everybody who saw this on Dental Town.
I posted a message about a similar case previously. This time I took pictures. The patient came in with very painful abscess in relation to cracked root of tooth#8.

I removed the tooth and found that there was no-buccal bone at all.

I used first my Er:YAG and then my Nd:YAG in the socket and then augmented the site with demineralised freeze dried bone.

The patient returned after 60hours for a follow up. She had been wearing a flipper during this period.

Inspection of site after removal of plate.

Any thoughts?
Take care
Etienne
gmclaurinSpectatorI have some questions. Why did you use your Er:YAG and then your Nd:YAG and on what settings? It looks like you did not have a need to cover your bone graft, so you just placed the flipper over the site?
Did you do any biostimulation, pain meds, antibiotic? It looks great! You said that you have done this before – how did that turn out?Thanks for all the details – Gail
etienneSpectatorThanks for the comment Gail
I used the Er:YAG to disinfect the site. The Nd:YAG with its deeper penetration was used to initiate clotting, biostimulate the tissue and further disinfect the site. The Er was used at 10Hz 350mJ, the Nd:YAG was used at 10hZ 100mJ if my memory serves me correctly. I have the settings at work somewhere ;)) Yes, I just placed the flipper. A membrane certainly wont hurt though. I did give the patient some pain meds, she didn’t use any though. I wasn’t taking chances with the infection so she took 1000mg Augmentin b.d. Ideally the patient should start with the AB 1 day pre-op though.The other cases turned out about the same as this one. 1 Patient removed her flipper during the first 24 hours and the graft didn’t look quite as nice as this after 48 hours. The combination of the Er and Nd:YAG seems to be quite effective.
The determing factor will be when I go in to place the implant. I’ll evaluate again in two weeks time.
Take care
Etienne
etienneSpectatorHi Guys
I saw this patient for her follow up prior to placing the implant. The restorations on the adjacent teeth were done after taking these pics.
Take care
Etienne
Glenn van AsSpectatorLooks marvelous and this is exactly what I love to see with the laser forum, a great case that we all see from time to time in the office and how lasers can be integrated into the whole process.
Well done Etienne, what is the treatment plan long term for the missing tooth.
Cya
Glenn
etienneSpectatorHi Glenn
Thanks for the compliment. I actually placed the implant last Friday. Unfortunately I have had a problem with my notebook and lost the pictures but will take new ones when I see her again. I have also placed a temporary crown on the implant this week. I think it turned out well. Sure beats waiting for the site to heal and then augmenting with symphysis or retromolar area bone!I have done some reading on PRP and believe that it will be even better for immediate augmentation of sites such as these. Especially if used in conjunction with BMP. Can’t wait for my next case…;))))
Take care
Etienne
Robert Gregg DDSSpectatorEtienne,
I wouldn’t waste you time with the PRP. Stick to your FRP Nd:YAG and you have all that you need. I’d use the same for dis-infection of the site.
Very nice result.
Bob
etienneSpectatorHi Bob
Thanks for your note. I recall a picture that I saw of a case that you used the Nd:YAG alone to initiate clotting and that sure seemed like it created a very nice “scaffold” for healing.I have not been able to get that kind of results. I still lose alveolar height when not using some kind of augmentation material. The demineralised freeze dried bone works OK but it is not ideal. Last night I did my first case with PRP after doing my normal laser procedure. The idea is to limit interventions at a later stage by trying to optimize the site at time of extraction.
The PRP product I used is actually a very interesting product. It is something bought of the shelf that is actually manufactured for use by the medical guys and has a shelf life of 3 years. They claim that the growth factors stay viable all this time…
Would be interesting to see how it turns out.
Take care
Etienne
Robert Gregg DDSSpectatorHi Etienne,
Exactly what is PRP that you are referring to?
I’m familiar with “Platelet Rich Proteins” as extracted from a patient’s blood…..
Thanks,
Bob
etienneSpectatorHi Bob
“PRP” is platelet rich plasma. I assume that is what you meant. It is extracted from blood, but not necessarily the patients own blood. The product that I used now is prepared from donor blood and frozen and therefore has the 3 year shelf life that I mentioned. Some people add BMP (bone morphogenetic proteien) to it to enhance the bone regeneration properties. The idea is to concentrate the growth factors in the wound area and also in this case, to create a scaffold for regeneration of bone.
Take care
Etienne
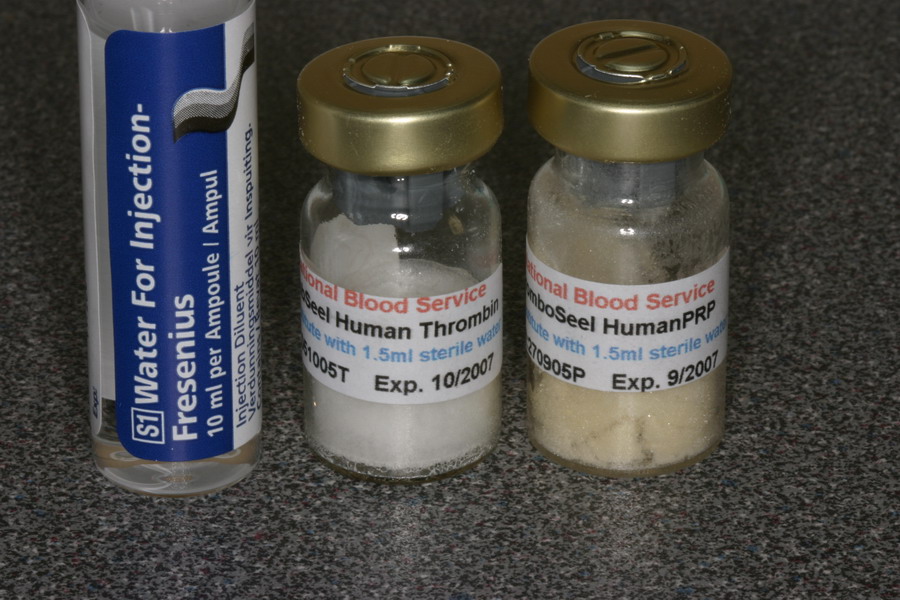
etienneSpectatorHi Guys
I did not think that this warranted another thread. Here is a case that I did today with laser and PRP, just as a matter of interest.This what the product look like.
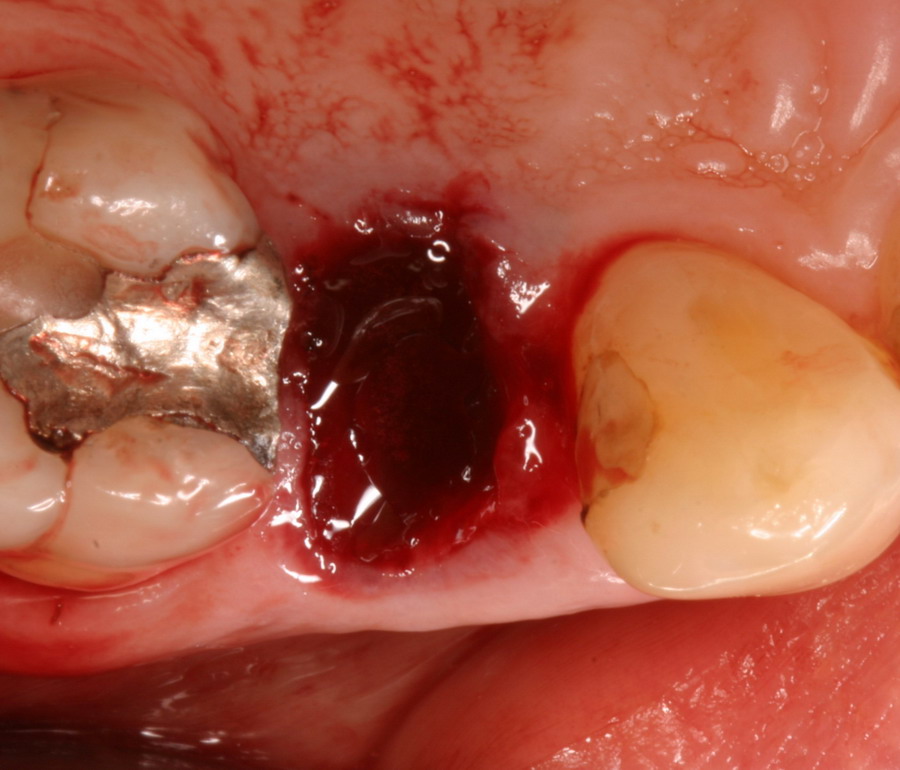
This was the case before I started.

After the root was removed I used the Nd:YAG inside the socket.
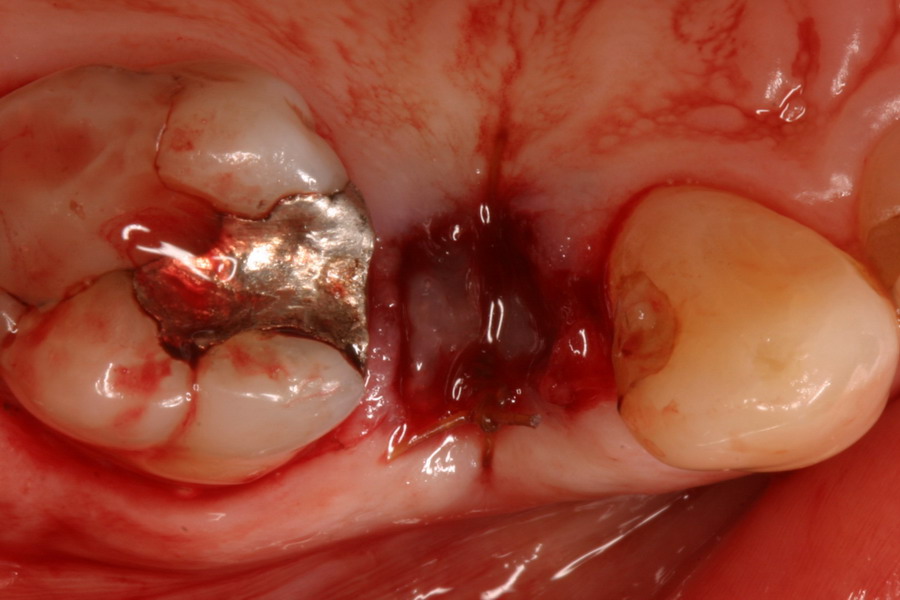
This what the clotted PRP and Thrombin looked like.

Here is the socket augmented with the clotted PRP and stabilized with a suture.
Any thoughts appreciated.
Take care
Etienne
arrowsmithSpectatoretienne,
The previous case with #8 being lost, adding a graft, and then placing the implant . . . . how long did you wait until placing the implant after the extraction and grafting? Maybe I’m wrong, but it looks like around a month . . . . do you think the buccal bone is stable enough? Did you reflect a flap during the placement of the implant? What size implant did you use?
Bob, there is a lot of discussion about atraumatic extractions preserving the bone height/levels. Is there any connection with using the Periolase to disinfect/clean the extraction site, and maintaining even more bone, long term?
aaroN
mkatzSpectatorThromboSeel – I’d love to get additional information… price, source, research data comparing its efficacy with fresh prepared PRP… any advice?
etienneSpectatorHi Aaron
I’ll check the exact dates from extraction till implant for you on Tuesday. I didn’t reflect a flap, used a one stage procedure with a 5mm X 13mm Co-Axis implant from southern Implants. Ideally I would have waited a bit longer but was afraid of bone loss.Bob knows more about this than I do but with initiating blood clotting with the Nd:YAG in the socket you get a beter scaffold for bone regeneration and thus maintenance of the alveolus. Long term, the bone will still recede of course, but this should give you time to get the implant in.
The idea with the PRP as well as the laser is to try to go one step further, especially in large defects. For smallish defects the laser alone should be sufficient.
Take care
Etienne
etienneSpectatorHi MKatz
Thromboseel is produced by the South Africa blood transfusion service form a select group of donors that are tested every 6 weeks. The product is only released after the donor has tested negative at a subsequent screening 6 weeks later.I’ll try to get some details for you regarding your questions.
Take care
Etienne -
AuthorPosts
