Forum Replies Created
-
AuthorPosts
-
Glenn van AsSpectatorHi folks: I really am enjoying pushing the envelope. I posted this on DT but not everyone goes there so here it is for you.
Hope its interesting
Glenn
Hi folks, this is NOT one of my patients but a dentist friend of mine referred this nice lady to me. She is on aspirin, mid 60s and is self conscious about her smile because of the differences in height of the tissue levels.
I see her today for the first time and advise her that I can do some gingival recontouring but due to the differences in height I will have to remove some bone as well.
Here is the sequence quickly and the rationale and the photos will help you see what I did.
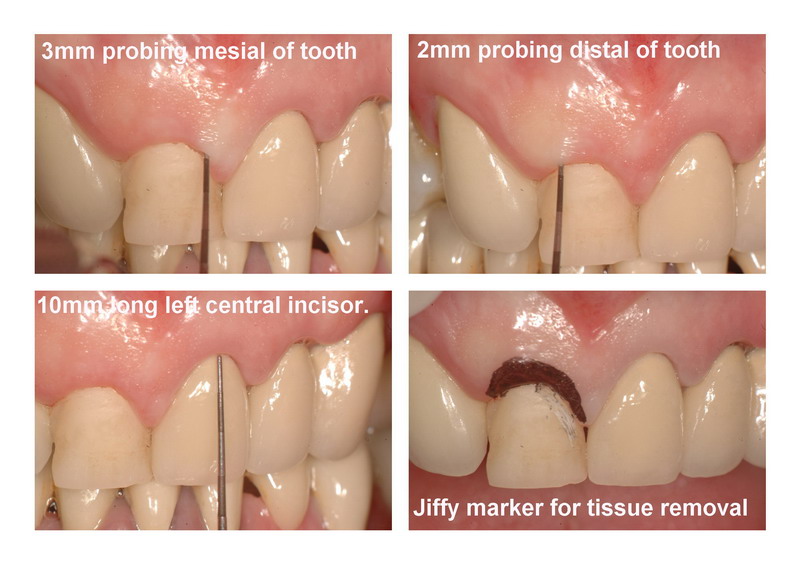
I had LOTS of attached tissue, but only 2-3mm of probing so in order to get the recontouring to stay (I had to take 3 mm off) I needed to remove bone.
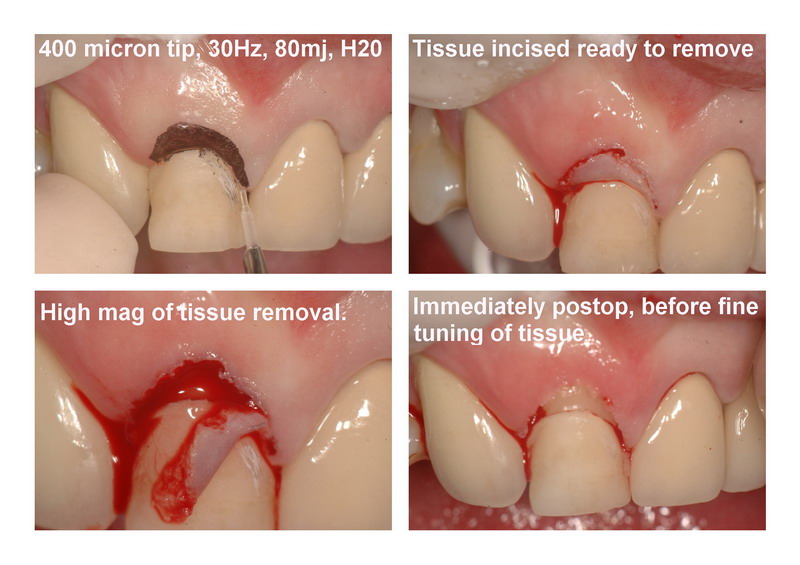
I marked the tissue with a jiffy marker to approximate the removal I needed. I did this with a 400 micron tip with air and water for arguments sake and got some bleeding which I coagulated with astringident. The patient was unaware that the tooth had a provisional temporary crown on it. I told her the edge of the tooth would be visible after the procedure and that a new crown would be needed at her dentists office.
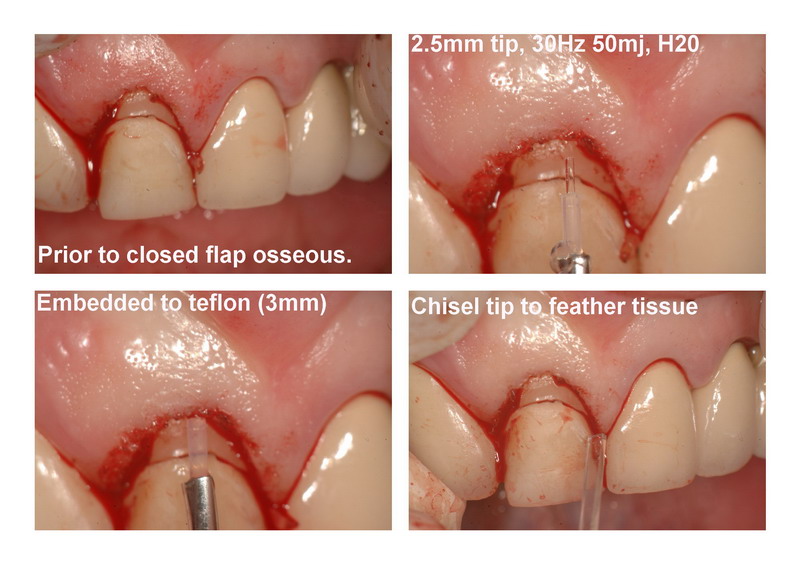
After the removal of the tissue I took a 400 micron tip (2.5mm to the teflon coating) and closed flapped the tip tactile method to remove bone. I also used the broader chisel tip to again go closed flap after the initial troughing was done.
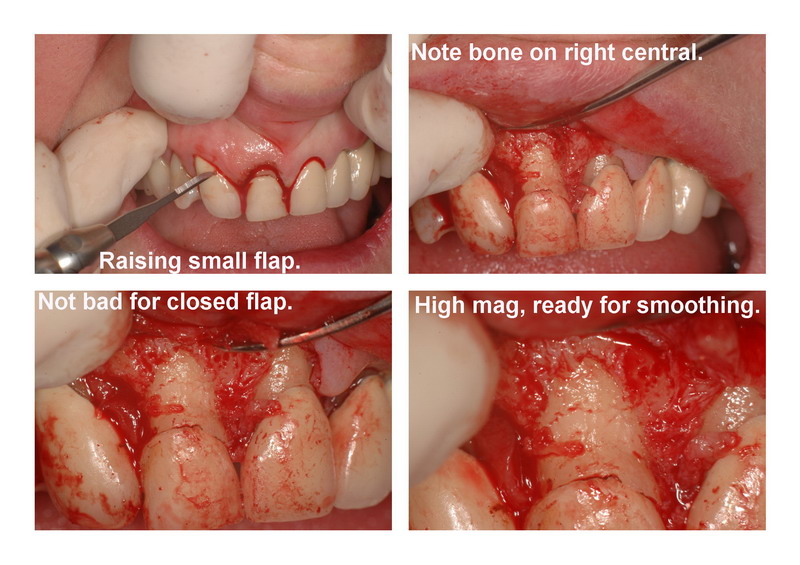
Then I raised a flap to see how I had done. Now it wasnt perfect but to my surprise I had done a decent job blindly doing this using the two tips when I compared the bone on the two centrals. I didnt use vertical incisions but my technique is slowly getting better. This took me about 50 mins with all the photos.
I used 6-0 sutures to tie up and was pretty pleased with the result. I think the patient liked it as well.
Anyways here are the photos, kinda neat to see the before and afters.
Glenn



Andrew SatlinSpectatorWay to go Glenn!!!!!
Now that wasn’t so bad right?
Soon your going to have to take back all those black triangle, root sensitivity and lets extract and place an implant comments. You are doing surgical periodontics.
Just joking of course.
Very nicely done!!! Great before and after documentation.
I would have handled this case the same way!
Thanks for sharing.
Andy
ASISpectatorHi Glenn,
Excellent handling! Great usual documentation of high standard again. Which camera is this now?
Did you have to recontour the osseous level to #21 upon flap being raised, as in one photo it appeared #11 was more apical than #21?
Very very nice.
Now that a respectable osseous relief has been shown that it can be achieved closed, the question then becomes: Will the routine approach be closed or open in a similar tissue biotype and alveolar process configuration?
Thanks for posting, Glenn.
Andrew
Glenn on the roadSpectatorHi Andy….thanks and I take back all the dark triangle , root sensitivity, implant comments now that I am a board certified periodontist…….ah wait a minute……….
GRIN
I feel this distressing need to start reading Pubmed to look at abstracts and research!!
Nah , just joking! Thanks for the comments but I still feel like that I should be doing things differently in certain areas but I will try to get Danny to give me a few more tips.
I appreciate all the help that you and Hack gave me in Vegas at Bobs meeting and if I have any degree of success it is through the learning I have done here from others cases.
Andrew!
Hi there, well I looked at the photos, the first photo the flap is not raised high enough and what you are looking at is part of the soft tissue , not actually the root. I never touched the 21 (left central) just the right one. I tried as Danny mentioned to make the two symmetrical. There was 3mm of soft tissue at the end over the bone.
I think that for now I will continue to raise flaps and see if I can figure out when it is ok to do closed flap and when it isnt and maybe I will post photos for Danny and Andy and Hack to look at and see if they see big errors that I created from the closed flap. Low low low settings and the chisel tip seem to make a big big difference.
Anyways, hope that is what you wanted to hear and I look forward to chatting with you soon. I have a BIG big surprise ready for the March 23rd VLG meeting (actually 2 surprises for the office) but you are going to have to be here to know what they are!!
GRIN
Cya and thanks for all your kind words and friendship.
Glenn
Glenn on the roadSpectatorHey guys…..I look forward to seeing you up here for the VLG meeting April 29th, and we have one study club meeting on March 23rd, 2005 in my office.
Paul, I am going out of town and having surgery but I have two very big surprises for you when you get here for that day.
Tell the rest of the group that they dont want to miss this meeting, its a secret what I have been able to accomplish but we will have a surprise guest, and in addition another surprise for that day.
Glenn
drnewittSpectatorHey Glenn
We will be thinking of you through the surgery. I will make sure the 23rd is set up and silky smooth and am looking forward to the surprises!
I was out with Jay tonight and not even a beer could loosen him up to give away the surprise. Looks like with surprises on the 23rd and some big ones at the April 29th Convergence meeting its a great time to be a VLG member!
drnewittSpectatorThis news item came accross my newswire accunt the other day. First I had heard about it. Anyone know whats going on?
The FDA Enforcement Report is published weekly by the Food and Drug Administration, Department of Health and Human Services. It contains information on actions taken in connection with agency Regulatory activities.
PRODUCT
Waterlase MD, dental laser unit, Model #6200218. Recall # Z-0543-05.
CODE
Serial Numbers: 10500210 to 10502680,inclusive.
RECALLING FIRM/MANUFACTURER
Biolase Technology, Inc., San Clemente, CA, by firm representative visit, on January 17, 2005. Firm initiated recall is ongoing.
REASON
Reports that the Waterlase MD, a dental laser unit, water bottle broke under pressure during installation.
VOLUME OF PRODUCT IN COMMERCE
209 units.
DISTRIBUTION
Nationwide and Internationally.
lookin4tSpectatorIronically, a hygienist just hyped this course word for word in some parts on dentaltown.
Just like at DT, no response to replies.
dkimmelSpectatorI think we all like to hype having a great experience. Too often we take a course and find it to be a waste of time or come away with one helpful hint.
Hopefully Tom will drop back in and let us know the rest of the story.
CE has become expensive in not just cost but time out of the office. That is one of the great things about this forum. We all share and learn from each other.
Robert Gregg DDSSpectatorQUOTEQuote: from N8RV on 6:09 pm on Mar. 7, 2005
And I’ve seen that ‘Vette, too. Real purty red one! (I’m still dealing with 6-speed envy … I got an automatic instead and can’t stop kicking myself for that.)She ever let you drive it, Bob?
— Don
Only if Janna chaperones!! :confused:
2thlaserSpectatorHey everyone,
Just wondering how everyone is using their laser for endo, Er, especially? Bob, Nd YAG? Can we share some thoughts? I have some ideas, and kind of want to begin a study on minimally invasive endo, which I think the laser needs to be a part of…From Mark on the Road back home!
Mark
AnonymousSpectatorMark, maybe by the overwhelming response, they’re not using the erbium much in endo
 ? 😉
? 😉What kind of study are you proposing?
Tom DaviesSpectatorTo answer some of the questions about my original post:
1. I think Janet’s protocol is mainly aimed at decontamination; however, de-epithelialization is occurring concurrently. Elimination of the bio-film in the perio pocket is the ultimate goal.
2. We have yet to see any patients back for 6 week therapy/re-evaluations, so I cannot report on any hard results yet.
3. This is being done by the hygienist, so there is no flap elevation. First visit you tackle the worst pockets or areas showing the most signs of disease. Microultrasonics, irrigation, diode laser. This may not necessarily be a quadrant; it could be two molars in two different quads. Next appointmnet, go to the next area or quad, treat that area, and re-lase the worst pockets from appt. #1. Continue until all teeth treated, then have 6 week therapy, re-evaluation.Janet’s training was great, and the cynic who posted the blast is a foul ball.
dkimmelSpectatorMark, 100% of the time I will use the Waterlase as a last pass in the canal staying 3mm short of the apex .
Sometimes I will use the Waterlase to start my access just getting into the dentin or getting to the pulp chamber. I will then use burrs as I have a hard time getting a proper access without a tactile sense. ( Through the scope may change this)
Only once have I done endo without numbing the patient on a vital fractures tooth.Hope that helps
marc andre gagnonSpectatorWe now follow theses cases since near a year
I received a lot of documentation from kavo in england
We are few dentist in canada than use the healozone
I prepare some courses about healozone in quebec
I use healozone for decay under 40 on diagnodent
root desensibilization
before bleaching
after bleaching
herpes
before crown cementationThe reason is simple, the hygieneist can use the machine in quebec
I send more photo laterbye
-
AuthorPosts
